Radiology:评价冠脉部分血流储备,哪种方法更好呢?
2018-01-28 shaosai MedSci原创
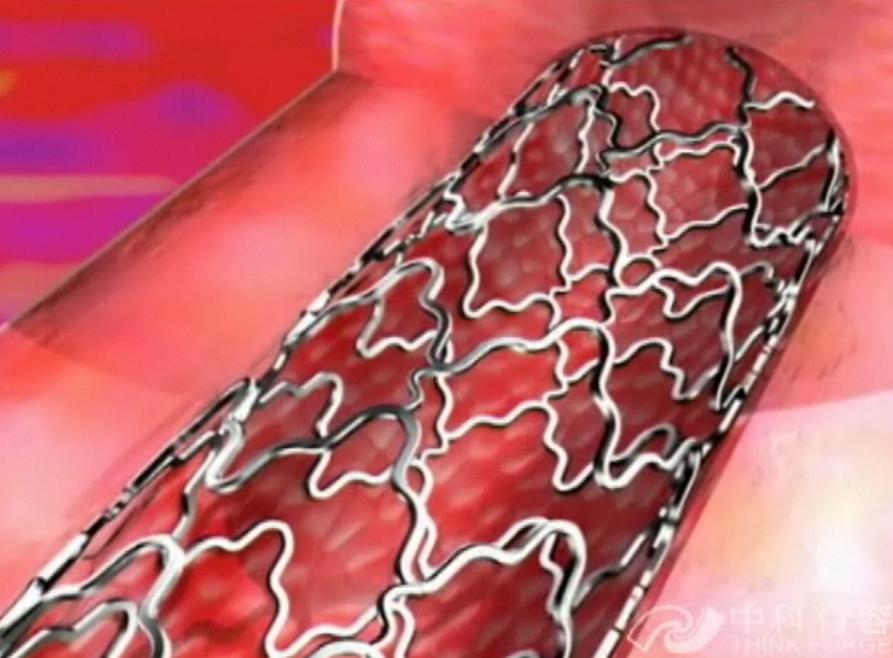
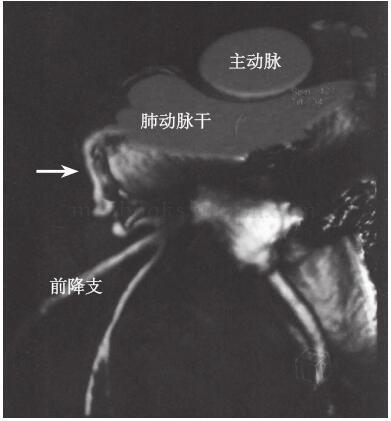
本研究旨在比较不同CT部分血流储备(FFR)算法对病变血管评价的诊断准确率,并将结果发表在Radiology上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









谢谢.学习了
53
#评价#
23
评价冠脉部分血流储备.
49
很有用
56
学习了提高了
48
学习了很有用
71
谢谢分享学习了
23
是很好的学习材料.不错.以后会多学习.
21