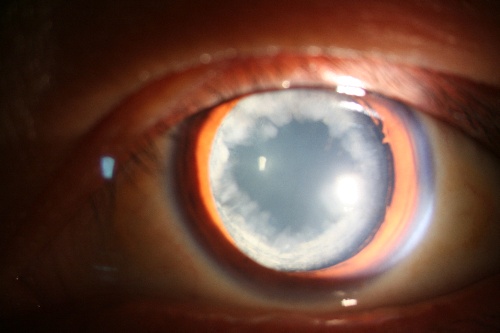
J AAPOS:25G经结膜免缝合玻璃体切除术是治疗先天性婴幼儿白内障中的良好选择!
2017-09-14 cuiguizhong MedSci原创
巴西圣保罗联邦大学医学院先天性白内障科眼科的Tartarella MB近日在J AAPOS发表了他们团队近期的一项工作,他们研究了25G经结膜免缝合玻璃体切割系统术中术后并发症的发生率。
巴西圣保罗联邦大学医学院先天性白内障科眼科的Tartarella MB近日在J AAPOS发表了他们团队近期的一项工作,他们研究了25G经结膜免缝合玻璃体切割系统术中术后并发症的发生率。
他们进行了回顾性研究,回顾了12岁以下先天性白内障患者进行25G经结膜免缝合玻璃体切除术的病历资料。对术后第1,7,10,15,30,60,90天及其后每3个月的复诊结果进行研究,并分析了视力敏感性结果和术中并发症的发生情况。

他们总共研究了44例婴儿的72只眼,其中28例(64%)患有双侧白内障。随访时间的中位数为28个月(范围12-93个月)。 47例眼(81%)手术后视力得到改善。有9例(13%)术后发生不良事件。有14例(19%)眼睛发生术后并发症:其中有6例眼睛(8%)出现继发视轴不透明,有6例(8%)眼睛出现继发性青光眼,1例(1%)眼睛出现后眼粘连,1例(1.4%)眼睛出现视网膜脱离。
因此,他们认为,25G经结膜免缝合玻璃体切除术是一种用于先天性白内障治疗的微创技术。在81%的眼中没有观察到术后并发症,其视力也得到显着改善。这为临床眼科医生治疗先天性白内障提供了借鉴。
原文出处:
Tartarella, M.B. and J.B. Fortes Filho, Twenty-five-gauge sutureless lensectomy in infants with congenital cataract. J aapos, 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
25
#AAP#
26
#25G经结膜免缝合玻璃体切除术#
27
#玻璃体切除术#
32
#婴幼儿白内障#
31
#先天性#
0
#玻璃体#
20
#5G#
19
谢谢分享.
22
学习了受益匪浅
27