NEJM:急性胰腺炎Cullen征和Grey-Turner征-案例报道
2015-12-10 chenshuo译 MedSci原创
男性,63岁,以往无酗酒史,今因突发性上腹部剧烈疼痛来院就诊。抽血检验结果显示,血清脂肪酶水平升高(1380U/L;正常范围为22-51U/L),与急性胰腺炎的诊断标准一致。
男性,63岁,以往无酗酒史,今因突发性上腹部剧烈疼痛来院就诊。
抽血检验结果显示,血清脂肪酶水平升高(1380U/L;正常范围为22-51U/L),与急性胰腺炎的诊断标准一致。
腹部超声检查显示胆囊和胆总管未见结石迹象。
随后,该男子接受静脉补液、应用止痛药以及胃肠减压等一些支持性的治疗来延缓病情。2天后,该男子因病情恶化被紧急送往ICU。
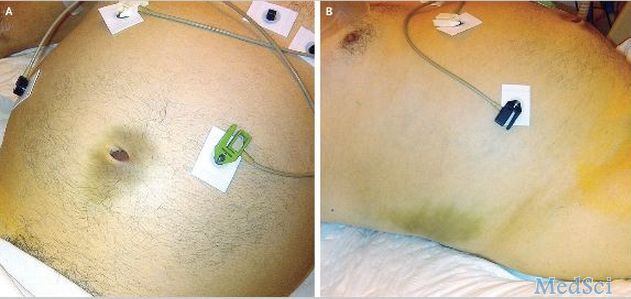
转院前,再次体格检查评估,发现该男子开始出现全身黄疸现象。同时,还出现了腹胀和脐周及腹部右侧出现了瘀斑(Cullen征、特纳氏征;如图A和B所示)。
血液检验结果显示血清总胆红素水平升高(4.2mg/dl[ 71μmol/l];正常范围,0.06-0.99mg/dl[ 1-17μmol/l])。
在后期的治疗中,CT检查结果证实该男子患上了急性坏死性胰腺炎和胰周积液的存在(Balthazar CT分级:E级),以及发现有胆囊结石的迹象。
不久,该患者开始出现多器官系统衰竭,尽管加强治疗和护理,最终病人死于并发症。
Xavier Valette, M.D,and Damien du Cheyron, M.D,Ph.D.Cullen’s and Grey Turner’s Signs in Acute Pancreatitis.N Engl J Med 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










第一次见到这个体征,简直是死亡阴影
115
是一篇不错的文章
108
值得进一步关注
118
不错,赞一个
104
这篇文章有一定深度
54
好杂志好文
68
好文章,学习了!
81
以前看过但没有影像资料
73
长见识
94
好文章,值得看。
82