【一般资料】
患者男,6岁
【主诉】
因左侧下颌后牙咀嚼痛10d来我院就诊。
【现病史】
年前左下后牙因龋损于外院行“充填治疗”10d前出现自发性持续性痛,咀嚼时疼痛加重。
【体格检查】
36牙合面见白色充填物,边缘不密合,周围见大量腐质,探痛(-),冷水反应(-),叩痛(+),无松动,牙龈无充血水肿。
【辅助检查】
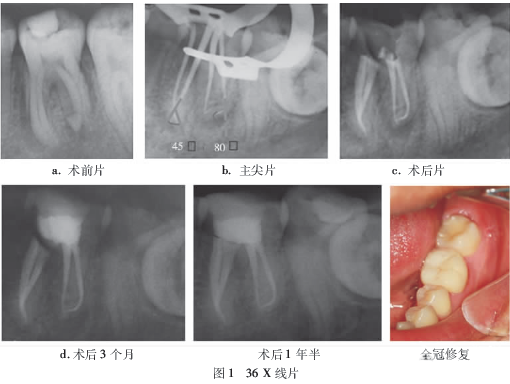
X线片可见36近中根牙周膜间隙增宽,远中根严重弯曲,有0.3cm×0.2cm椭圆形低密度区,边界不清。
【初步诊断】
36慢性尖周炎。
【治疗】
6根管治疗术后行全冠修复。36置橡皮障,常规开髓、揭髓顶,超声工作尖(ETBD)去除牙本质领,探及5个根管口,10C锉疏通MB、ML、DB根管,#8C锉疏通DL和MM根管,测量工作长度(MB:20mm,ML:23.5mm,MM:22.5mm,DB:21.5mm,DL:22.5mm),PathFile初预备根尖至#19,MB、ML、DB根管ProTaper预备至F2,DL、MM根管Mtwo预备至#25。预备后,发现MM与MB融合为1个根管(2-1型)。52.5g/LNaCLO+30mL/LH2O2交替冲洗,超声荡洗,封Ca(OH)糊剂。1周后复诊,自觉症状消失,无渗出,主尖拍片(牙胶尖预弯处理)并按照Schneider法测量弯曲度,用AH-Plus糊剂热牙胶连续波充填。X线片示36根管恰填。术后3个月复查,远中根根尖周围骨密度较术前增高,根尖周病变正在愈合。1年半后复查,尖周病变基本消失,行全冠修复。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#下颌#
26
#根管#
41
#磨牙#
40