经桡动脉逆行导丝处理左前降支(LAD)完全闭塞(CTO)
2012-02-04 傅国胜 MedSci原创
病例简介 患者男,67岁,因“反复活动后胸痛7月余,加重2周”转入我院;既往高血压病35年,无糖尿病,不吸烟。入院心电图显示窦性心律,V1~3异常Q波;心脏超声显示左心室射血分数(LVEF)62%,左室舒张末期内径(LVEDD)55 mm;血肌钙蛋白(-);当地医院冠脉造影(CAG)提示左主干(LM)中段起50%~60%狭窄,左回旋支(LCX)正常,左前降支(LAD)起始处完全闭塞(CT
 |
 |

病例简介
患者男,67岁,因“反复活动后胸痛7月余,加重2周”转入我院;既往高血压病35年,无糖尿病,不吸烟。入院心电图显示窦性心律,V1~3异常Q波;心脏超声显示左心室射血分数(LVEF)62%,左室舒张末期内径(LVEDD)55 mm;血肌钙蛋白(-);当地医院冠脉造影(CAG)提示左主干(LM)中段起50%~60%狭窄,左回旋支(LCX)正常,左前降支(LAD)起始处完全闭塞(CTO),右冠脉近中段40%~50%病变,通过锐缘支及右冠脉后降支(PDA)远端对LAD提供侧支循环。
前向、逆向选择
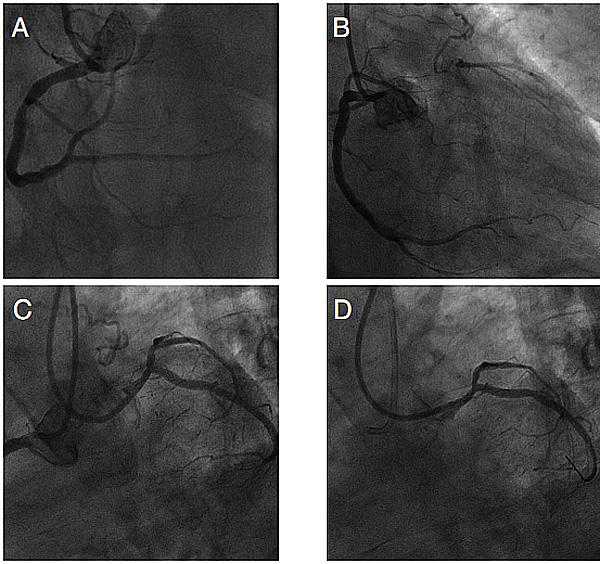
CAG结果如图A~E。该患者病变虽累及LM,但仅LAD完全闭塞,患者相对年轻,心脏收缩功能基本正常,如不能开通LAD,可考虑冠状动脉旁路移植术(CABG)。
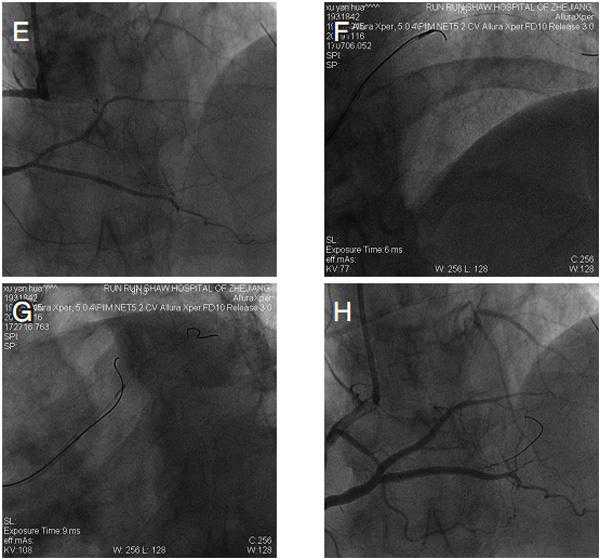
由于LAD起始不明确,选择前向还是逆向技术值得讨论,常规血管内超声(IVUS)检查可清楚看到前降支闭塞段起点,我们用IVUS证实导丝进入LAD,但方向调整困难(图F、G),遂放弃前向改逆行导丝技术。
送入导丝
在微导管支持下,Fielder导丝经后降支到间隔支,未发现明确可用侧支进入LAD远端(图H)。造影提示锐缘支有远端和近端2个分支进入LAD,远端分支有明确的大迂曲,估计导丝无法通过,近端分支虽有一直角转弯,但之后无明显迂曲,故选择近端分支。
导丝无法通过LAD闭塞远端病变,改用Crosswire-NT,虽能走向LM,但始终无法进入真腔,估计与LAD起始处严重成角有关,故将导丝努力操作至LCX进入真腔,但似乎不能将导丝送至LM。我们试图将一硬导丝和IVUS导管送入中间支,“挺直”LAD与LM成角,仍不能将导丝送入LM。后试图将逆行导丝锚定在LCX,再将微导管送入LM-LAD/LCX分叉,但无法通过病变。最后我们决定用球囊低压扩张封堵LCX开口,终将逆向导丝送至LM并进入前向GC。锚定逆向导丝操作微导管进入前向指引导管,交换成Fielder FC 300导丝,采用Back-end技术扩张闭塞血管。因逆向导丝过于靠近闭塞远端血管,故从前向顺利送入导丝,而撤出逆向导丝。
支架置入成形
由于病变为前三叉病变,LCX在逆向操作导丝时有明显损伤,有双支架指征,故决定采用反向Culotte技术,先后于LM-LAD置入3.0 mm×28 mm和LMo-LXCX置入3.5 mm×33 mm支架。经6F前向指引导管送入3.5 mm×15 mm和3.25 mm×15 mm高压球囊,经逆向指引导管送入导丝及2.0 mm×15 mm球囊行3球囊成形。
效果
左冠脉(LCA)血流Ⅲ级,未见侧支血管损伤。IVUS 确认支架膨胀贴壁良好。术后3日出院,出院后无心绞痛发作,术后1年复查CAG无明显内膜增生。
■治疗体会
对开口部位不明确的完全闭塞病变,IVUS对前向技术有重要指导意义;对类似病变也可采取直接逆行导丝技术;经心外膜侧支血管行逆向导丝技术可行,但术后监测非常重要;经双侧桡动脉行闭塞病变逆行导丝技术和6F指引导管行LM介入安全可行,且在造影剂用量、改善患者生活质量等方面有较大优势;在处理复杂非常病变时,如需要3或4球囊对吻成形,可采用双指引导管技术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








谢谢分享
0
#经桡动脉#
33
#CTO#
43
#导丝#
37
#桡动脉#
24