J Dent:X线检查龋齿效果可靠吗?
2015-04-15 sunshine 译 MedSci原创
J Dent:X线检查龋齿效果可靠吗?关键词:颌翼片 龋齿 牙齿 放射线显影术本次系统性回顾的目的是为了评估影像学方法检测不同牙齿的不同部位龋坏的准确性。分别在临床上和体外研究X线检测乳牙自然龋坏的准确性(特异性/灵敏性)。使用 QUADAS-2来评估偏倚风险,使用随机效应荟萃分析计算总得敏感性、特异性以及诊断比值比(DORs)。分别分析牙齿咬合面龋
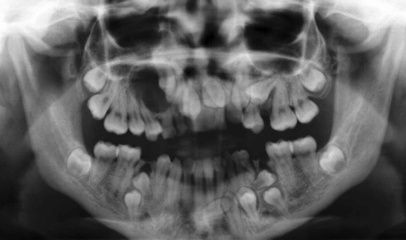
本次系统性回顾的目的是为了评估影像学方法检测不同牙齿的不同部位龋坏的准确性。
分别在临床上和体外研究X线检测乳牙自然龋坏的准确性(特异性/灵敏性)。使用 QUADAS-2来评估偏倚风险,使用随机效应荟萃分析计算总得敏感性、特异性以及诊断比值比(DORs)。分别分析牙齿咬合面龋和邻面龋,牙本质龋以及已形成龋洞的牙齿,进一步区别不同的病损。
研究查阅确定了947篇文章,分析了442篇全文。本次分析纳入了117例研究(涉及13375颗牙齿,19108个牙面),大部分研究是关于恒牙,且具有较高的偏倚。任何一种病变(如初始病变)的检测敏感性都很低 (总 DOR [95% CI]: 0.24 [0.21/0.26] to 0.42 [0.31/0.34]),但是特异性却达到了中度到高度 (0.70 [0.76/0.84] to 0.97 [0.95/0.98])。牙本质病变检测的敏感性较高 (从邻面龋的0.36 [0.24/0.49] 到咬合面龋的0.56 [0.53/0.59] ),特异性在0.87 [0.85/0.89]到0.9[0.94/0.96]之间。没有关于咬合面已形成龋洞的研究报导,对邻面已形成龋洞的研究显示,灵敏性增加了0.6以上,保持在0.9以上。对于邻面已形成龋洞的牙齿,X线检查是非常准确的,X线检查同时也适用于检测牙本质龋,在患龋率高以及龋易感的人群中,对于龋齿早期病变的检测,应当考虑更为灵敏的检测方法。
该研究的临床意义在于,X线检查尤其适用于检测破坏较多的病损,而且诊断假阳性的可能性较低。对于患龋率高和龋易感者来说,检测龋齿的早期病变,应当选择比X线检查更加敏感的检测方法。
原始出处:
Schwendicke F, Tzschoppe M, Paris S. Radiographic caries detection: A systematic review and meta-analysis.J Dent. 2015 Feb 24. pii: S0300-5712(15)00049-4. doi: 10.1016/j.jdent.2015.02.009.
本文系Medsci原创编译整理!转载需要先获得授权,并附原文链接。谢谢!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好文章,还会关注
54
有用
110
#X线#
24