【一般资料】
患者,男,71岁,
【主诉】
因发现左颌下肿物23年,近1个月渐增大于2010年12月13日来我院口腔科就诊
【体格检查】
老年男性,发育正常,神志清,检查合作。面部对称无畸形,左颌下区可触及一界限清楚肿物,大小约1.5cmx0.8cm,活动度好,质地稍硬,轻度压痛。
【辅助检查】
B超检查:左颌下腺实性肿块,大小1.5cmx1.0cm,界限清。右颌下、双侧颈部多发淋巴结肿大。
【治疗】
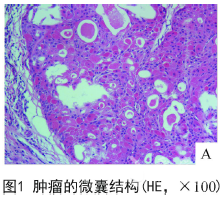
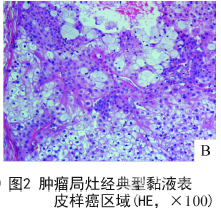
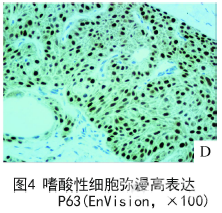
患者术前各项检查无异常后,于2010年12月17日全麻下行左颌下腺及肿物扩大切除术和颈部淋巴结清扫术。术中所见:肿物位于左颌下腺下极,质稍硬,边界尚清,与下颌舌骨肌部分粘连。完整切除肿物和左颌下腺,术后病理诊断为“嗜酸细胞性黏液表皮样癌”。患者术后恢复良好,患者术后行“注射用胸腺法新”皮下注射增强免疫治疗和定期复查,未行肿瘤化疗和放疗。随访患者62个月,未见肿物复发和转移。大体检查:类圆形肿物一个,大小1.5cmx1.0cmx0.8cm,切面未见明显包膜,为囊实性。以实性区为主,实性区约占肿瘤的95%。实性区灰白灰黄色,质硬。局部可见小囊腔,囊内容物为清亮黏稠液体。镜检:肿瘤主要由嗜酸性细胞构成,嗜酸性细胞呈“铺砖样”排列成巢状、片状和大小不等的囊腔结构(图1)。嗜酸性细胞体积中等大,呈多角形,细胞质呈颗粒状,丰富、红染。细胞核圆形,核仁明显。可见少许的经典型黏液表皮样癌(mucoepidermoidcarcino ma,MEC)的区域,该区域可见黏液细胞、中间型细胞和表皮样细胞,部分表皮样细胞胞质透亮(图2)。各种肿瘤细胞异型性小,不见坏死,核分裂相罕见。肿瘤中不见角化,不见血管和神经的侵犯。免疫组织化学染色,嗜酸性细胞表达抗线粒体抗体(antimitochondrialantibody,AMA)(图3)、广谱CK、EMA和P63(图4)。组织化学染色,嗜酸性细胞显示憐钨酸苏木素(phosphotungsticacid-hematoxylin,PTAH)染色阳性,胞质内见蓝染颗粒。

【讨论】
嗜酸细胞性黏液表皮样癌(oncocyticmucoepidermoidcarcinoma,OMEC)是MEC的一个特殊亚型,主要由嗜酸性细胞构成,约占MEC的2%。OMEC极为罕见,易被误诊为其他肿瘤。OMEC好发于成年人,发病年龄为20~79岁,平均57岁。男女发病率之比为1.25:1。OMEC最常累及的部位是腮腺,其他的部位有颌下腺、上腭、泪腺、气管、支气管、颈部和舌下腺等。巨检:肿瘤界限清楚,但没有包膜,切面为实性或囊实性。肿瘤大小1.2~6.5cm,平均大小2.6cm。组织学上,肿瘤主要由嗜酸性细胞排列成的巢状和片状结构构成,间质通常为硬化的胶原。嗜酸性细胞的特点是具有丰富的、嗜酸性颗粒状细胞质。细胞核圆形、居中,可见明显的核仁。同时,肿瘤中可见少许的经典型MEC的3种细胞,即表皮样细胞、黏液细胞和中间型细胞。嗜酸性细胞表达AMA、P63和CK。PTAH染色显示嗜酸性细胞阳性。OMEC多是低级别恶性肿瘤,其次是中级别OMEC,高级别罕见。OMEC治疗主要是肿物的全部切除和长期随访,术后一般不需要常规抗肿瘤治疗。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#表皮样#
32
#细胞性#
31
#颌下腺#
37
好资料学习了!
32