NEJM:早产卵巢过度刺激综合征
2015-06-12 MedSci MedSci原创
一名3个月大的女婴因会阴部出现肿胀,而来院就诊。经问诊,该女婴是一名早产婴儿,其在母体内孕育27周后即出生了,生后送至新生儿ICU观察75天因情况良好出院。出院不久,其母亲发现其外阴部出现红肿,并逐渐加重。体格检查发现,该女婴的外阴和阴蒂部位(如图A所示)出现肿胀现象,但其他部位无明显异常。实验室检查结果显示,血清雌二醇(310皮摩尔/升[ 80微克每毫升];婴儿正常范围值::20至40皮摩尔/升
一名3个月大的女婴因会阴部出现肿胀,而来院就诊。经问诊,该女婴是一名早产婴儿,其在母体内孕育27周后即出生了,生后送至新生儿ICU观察75天因情况良好出院。出院不久,其母亲发现其外阴部出现红肿,并逐渐加重。
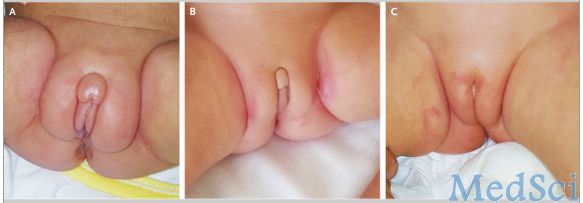
体格检查发现,该女婴的外阴和阴蒂部位(如图A所示)出现肿胀现象,但其他部位无明显异常。实验室检查结果显示,血清雌二醇(310皮摩尔/升[ 80微克每毫升];婴儿正常范围值:20至40皮摩尔/升到10微克每毫升)、促性腺激素促卵泡激素(17.2 MIU /毫升;正常范围值:0.5至2.4)和促黄体生成激素(4.7 MIU /毫升;正常范围值:0.01到0.21)。腹部B超结果显示,右侧卵巢囊肿。
早产卵巢过度刺激综合征是一种自限性疾病,无需治疗也能自愈。随后,该女婴定期随访,在没有进行任何治疗措施的情况下连续监测体内血清促性腺激素和雌二醇水平。
4周后,该婴儿体内血清雌二醇水平最高时达到每升700皮摩尔(每毫升190 PG),然后下降,雌二醇和促性腺激素水平逐渐恢复正常。第6个星期随访时,其会阴部和阴蒂的肿胀已大大减少(如图B所示)。第14周随访时,其会阴部已恢复良好。腹部超声再次检查发现其卵巢囊肿已经完全消失,但为了确保其已完全痊愈,该女婴在接下来的12个月内仍需定期随访。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














不错,赞一个
112
这篇文章有一定深度
109
是一篇不错的文章
107
值得临床关注
114
挺好
142
看看
104
早产男婴也有外阴肿胀现象
64
#综合征#
29
?
75
还真没见过
84