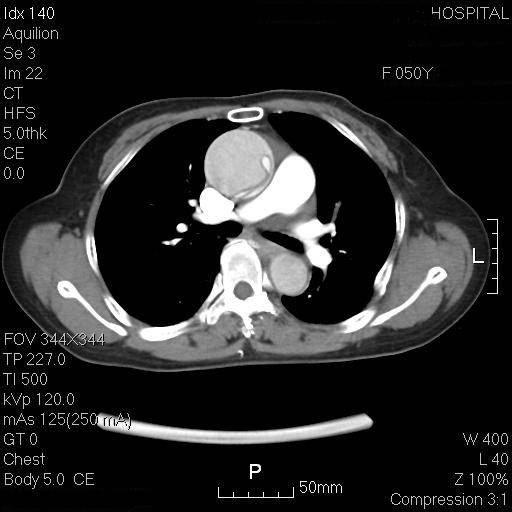
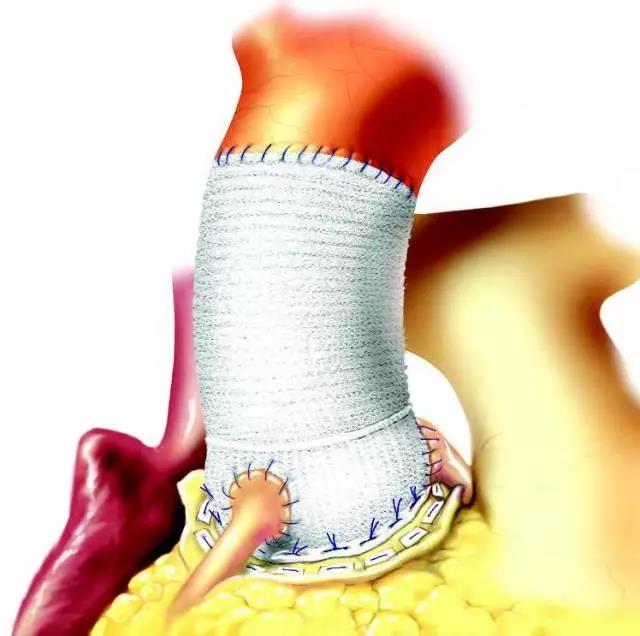
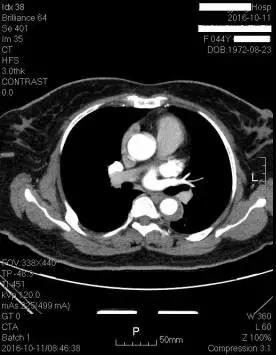
Sci Rep:B型主动脉夹层腔内主动脉修复术在中国的应用演变和疗效
2017-12-12 xiangting MedSci原创
2008至2015年期间,中国大陆进行的B型AD的TEVAR安全性比中国以前或西方国家的要好。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#B型主动脉夹层#
32
#修复术#
0
#腔内主动脉修复术#
24
#演变#
38
#主动脉#
26
#动脉夹层#
29
学习一下谢谢
40
学习.谢谢分享
49