Food Funct:富含甜菜红色素的仙人掌科(火龙果和仙人掌果)对于内皮和血管功能的影响:动物和人体研究的系统综述
2021-03-13 Dr.Sun Nutrition & Health MedSci原创
火龙果(量天尺属)和仙人掌果(仙人掌属)属于仙人掌科物种,已经在全球广泛使用,作为可靠的食物来源以及传统的民间疗法。由于其具有高水平的生物活性植物化合物,特别是甜菜红色素(betalain),它们最近
火龙果(量天尺属)和仙人掌果(仙人掌属)属于仙人掌科物种,已经在全球广泛使用,作为可靠的食物来源以及传统的民间疗法。由于其具有高水平的生物活性植物化合物,特别是甜菜红色素(betalain),它们最近引起了科学的兴趣。早期的系统综述已经研究了补充这些仙人掌类对于肥胖、2型糖尿病和心血管危险因子:体重和成分、血清甘油三酯类、胆固醇、血糖和血压的影响。然而,其对于血管健康和内皮功能的作用有待综述。
由于内皮层在调节血管紧张度(即通过内皮一氧化氮合酶通路)方面发挥着最终作用,同时控制白细胞在内皮炎症期间的招募,正常内皮功能的破坏可能导致内皮功能障碍——动脉粥样硬化发作的前兆和心血管事件的有用预测因子。


前不久,英格兰Food & function上发表了一篇文章,英国伦敦国王学院的研究人员进行了系统综述,评估了火龙果和仙人掌果在体内动物模型和人体研究中对于内皮和血管功能的生理作用。动物研究表明,血管舒张和血清一氧化氮可能增加,血管硬度和血压降低。少量的人体研究表明心率降低,以及心率变异性增加。

研究人员在以下数据库中进行了电子搜索:PubMed (MEDLINE)、EMBASE (via Ovid)、CINAHL、Scopus、Web of Science®、以及Cochrane Library (CENTRAL)。从起初至2020年1月以来,所有期刊都进行了检索,没有语言限制。感兴趣的结果是血压、动脉硬度、血管反应性和内皮功能障碍的生化标记物。两名调查员独立进行了研究选择和数据提取。在394个参考文献中,只有16项研究(9项动物和7项人体)符合选入标准。

系统性综述的范围采用PICOS(人群、干预措施、对照、结局和研究设计方案)的形式
总的来说,从营养学和方法学的角度来看,动物研究的证据相当薄弱,因为近一半的研究存在明显的缺陷并缺乏稳健性。
在人体研究中,有两项观察到仙人掌科对于血压的积极影响,这些研究只在普遍年轻范围(25-55岁)的患有冠状动脉疾病和2型糖尿病的人群中持续2至4周。这值得今后采取办法,在更长的时期内调查其对更广泛年龄组中更健康人群的影响。
虽然其中一项研究中没有实施对照,但使用的剂量是所有研究中在营养上最为现实的。他们的治疗是250毫升稀释仙人掌果汁饮料,只含有50克仙人掌扁茎。

体重、腰围、收缩压和舒张压的值在补充的某个点分别显示出显著差异
对患有冠状动脉疾病的男性进行的随机对照试验报告,利用从仙人掌果中提取的富含甜菜红素的提取物进行只有两周的干预,显著降低了收缩压(3.16 mmHg,p<0.0001)。与其他研究不同的是,给参与者的干预胶囊只含有甜菜红素(每粒胶囊25毫克)。这强烈地暗示,收缩压的改善可归因于甜菜红色素。

2周的治疗对研究变量的影响
另一个随机对照试验调查强化甜菜根的面包对健康男性个体24小时动态血压的急性影响。将对照面包与白甜菜根面包和红甜菜根面包对比,红甜菜根面包在摄入后0-24小时期间更有效地降低了舒张压(p<0.05)。从本质上讲,白甜菜根面包和红甜菜根面包在所有宏量和微量营养素上都相同,包括膳食纤维和硝酸盐(这也是一种强血管活性剂),只有甜菜红色素作为两者之间唯一的区别。这进一步强化了这样一种观念,即这些生物活性甜菜红色素可能在这些可食用仙人掌科的心脏保护作用中发挥重要作用。

摄入200克对照面包、200克强化了白甜菜根和红甜菜根的面包之后餐后收缩压和舒张压曲线下面积的平均变化
至于心率和心率变异性,在两个设计精美的急性随机对照试验中提供了相当有力的证据。研究人群是年轻(21-24岁)身体活跃的男性或职业运动员。由于这些是运动和表现研究,心率不可避免地会随着有氧运动而增加,因此心率在各组之间进行比较。Van Proeyen等人报道在治疗组食用仙人掌果提取物(OpunDia)后,心率每分钟降低10次,但没有提供相当于该提取物的成分或新鲜水果。这些结果与Schmitt等人的研究结果几乎相同,在他们的研究中,治疗组在食用了类似的仙人掌果提取物(相当于每个成年人300克新鲜水果)后,也每分钟减少9次心率。这种剂量可能看起来相当高,但仍在现实中可以实现的剂量之内。除心率外,治疗组的心率变异性也更高。在Khouloud等人中,他们的亚慢性运动试验在经过两周的干预后也取得了类似的改善。总的来说,心率和心率变异性是预测中风和冠心病的强大生物标志物。因此,可以公平地建议,补充仙人掌科可能有助于改善这种状况,尽管还需要做大量的研究来证实这一点。
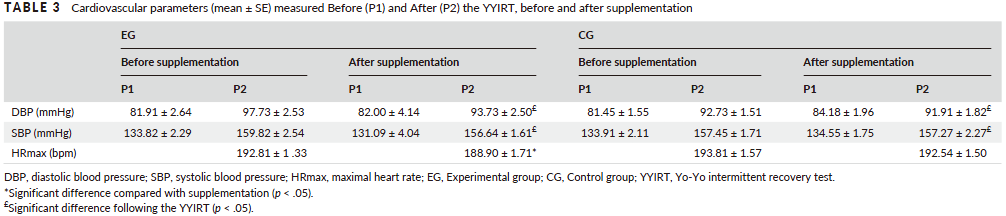
补充梨果仙人掌果汁前后Yo-Yo间歇恢复测试之前和之后的心血管参数测量
总体而言,研究对于血压的影响的全部5项动物研究报告了显著的降低,1项报告了血管紧张度改善,2项观察到血清一氧化氮升高,2项报告了动脉硬度降低。而在人体研究中,5项中只有2项发现血压降低,5项中有3项报告心率降低,唯一1项研究对于心率变异性影响的研究报告了显著增加。
总之,这次系统综述中提出的发现表明,尽管影响血压的证据好坏参半,但补充可食用的仙人掌科火龙果和仙人掌果似乎能改善血管和内皮功能。虽然动物研究的结果不太乐观,但人体干预试验提供了证据证明,这些仙人掌科改善心率并且增加健康和有心血管疾病风险人群的心率变异性。综合起来,这可能暗示了这些仙人掌科的潜在用途,作为改善血管功能障碍和其他心血管相关疾病的一种新型治疗选择。
原始出处:
Alex Cheok 1 , Trevor W George, Ana Rodriguez-Mateos et al. The effects of betalain-rich cacti (dragon fruit and cactus pear) on endothelial and vascular function: a systematic review of animal and human studies.Food Funct. 2020 Aug 1;11(8):6807-6817. doi: 10.1039/d0fo00537a. Epub 2020 Jul 27.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#色素#
44
#food#
41
#系统综述#
37
#血管功能#
40
关注一下
80
可以关注
70
比较有前瞻性的研究
80