Lupus:尿中性粒细胞明胶酶相关脂质运载蛋白可作为重度儿童狼疮性肾炎的生物标记物
2013-05-22 Lupus dxy
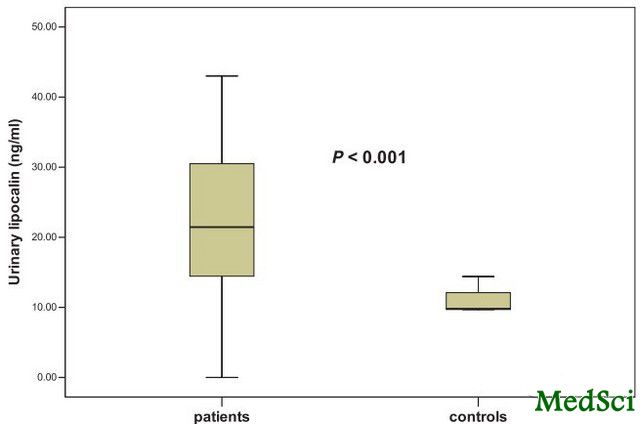
SLE患儿组与对照组相比,其尿NGAL水平明显升高 LN患者尿NGAL水平与系统性红斑狼疮病情活动指数中的肾脏积分相关 当尿NGAL/肌酐≥10.07ng/mg时,其预测III型和IV型LN的敏感性为91%,特异性为70% 超过60%的儿童系统性红斑狼疮(SLE)患者合并狼疮性肾炎(LN)。中性粒细胞明胶相关脂质转运蛋白(NGAL)是一种由白细胞在炎症状态下分泌的蛋白质,在缺血及损伤后

LN患者尿NGAL水平与系统性红斑狼疮病情活动指数中的肾脏积分相关
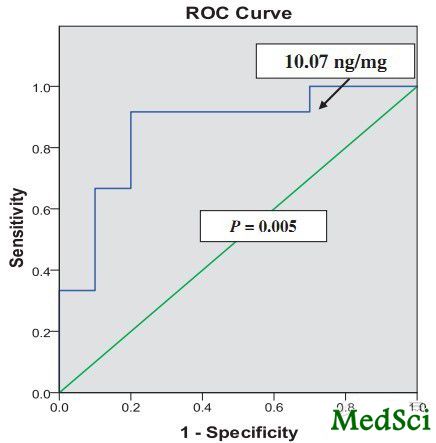
当尿NGAL/肌酐≥10.07ng/mg时,其预测III型和IV型LN的敏感性为91%,特异性为70%
超过60%的儿童系统性红斑狼疮(SLE)患者合并狼疮性肾炎(LN)。中性粒细胞明胶相关脂质转运蛋白(NGAL)是一种由白细胞在炎症状态下分泌的蛋白质,在缺血及损伤后的肾组织中高表达。为评估SLE患儿尿液及血清中的NGAL是否可以成为其肾脏受累的标记物,来自埃及曼苏尔大学儿童医院儿童肾病科的A Hammad等人进行了一项研究。研究结果发表于2013年5月的《狼疮》(Lupus)杂志上。研究认为尿NGAL是SLE患儿合并增殖性肾炎的一种敏感的生物标记物。
研究者评估了33例活动期SLE患儿(22例合并LN,11例不合并LN)的尿液及血清中的NGAL水平,同时与15例相匹配的对照组的相应指标进行对比。
与对照组相比,SLE患儿的尿液NGAL水平升高(P<0.001)。在合并LN的患者中,其尿液NGAL水平较不合并LN的患者更高(P<0.001)。合并LN患者的血清NGAL水平与对照组相比无明显差别(P=0.4),但其尿NGAL水平与系统性红斑狼疮病情活动指数中的肾脏积分相关(r=0.5,P=0.02),但与血清NGAL无相关性(P=0.5)。当尿NGAL/肌酐≥10.07ng/mg时,其预测III型和IV型LN的敏感性为91%,特异性为70%。
研究者认为,尿NGAL是SLE患儿合并增殖性肾炎的一种敏感的生物标记物。
Urinary neutrophil gelatinase-associated lipocalin as a marker of severe lupus nephritis in children.
INTRODUCTION
More than 60% of children with systemic lupus erythematosus (SLE) develop lupus nephritis (LN). Neutrophil gelatinase-associated lipocalin (NGAL) is a protein secreted by leukocytes during inflammation and is overexpressed in the kidneys following ischemic and nephrotoxic damage.
AIM
To study urinary and serum NGAL in children with SLE and investigate their possible role as markers of renal involvement. Methods Urinary and serum levels of NGAL were assessed in 33 children with active SLE (22 with and 11 without LN) and compared to 15 matched controls.
RESULTS
Children with SLE had elevated urinary NGAL as compared to controls (P<0.001). Levels of urinary NGAL were higher in patients with LN than those without LN (P<0.001). In patients with LN, serum levels of NGAL were not significantly different from controls (P=0.4) and urinary NGAL correlated with the renal score of the Systemic Lupus Erythematosus Disease Activity Index (r=0.5, P=0.02) but not with serum NGAL (P=0.5). Urinary NGAL was significantly predictive of class III and IV LN (P=0.005) with 91% sensitivity and 70% specificity to levels ≥ 10.07 ng/mg creatinine. Conclusions Urinary NGAL is a sensitive marker of proliferative nephritis in juvenile SLE.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#标记物#
25
#明胶酶#
40
#中性粒细胞#
38
#生物标记#
34
#生物标记物#
36
#狼疮#
31
#肾炎#
41