Heart:英国先天性心脏病患者的心脏或心肺移植
2019-01-13 xiangting MedSci原创
虽然预计CHD患者的移植会增多,但英国的实际数字似乎滞后于晚期心衰CHD患者的增多。
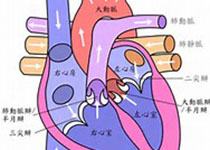
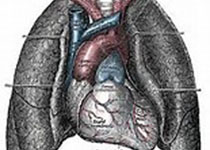
先天性心脏病(CHD)患者的寿命延长与晚期并发症相关,主要是心衰,这使得患者可能不适合重新手术并且药物治疗无效,因此转诊进行移植。这项研究评估了英国CHD患者心脏和心肺移植的当前作用和未来前景。
对英国1997-2015年的医院事件进行了回顾性分析,确定接受心脏或心肺移植的CHD患者(ICD-10'Q2xx.x')。
共有444例患者进行了469次移植(82.2%为心脏移植和17.8%为心肺移植)。一半移植患者的CHD复杂性为轻或中度,该百分比随时间而增加(p=0.001)。总体而言,随着时间移植越来越多,心肺移植的比例下降(p<0.0001),而成人移植比例保持不变。第1年的死亡率较高,尤其是心肺移植后,但此后死亡率仍然相对较低。老年人和心肺移植是死亡的强预测因子。虽然预计CHD患者的移植会增多,但英国的实际数字似乎滞后于晚期心衰CHD患者的增多。
目前和未来预测的CHD移植数量增多似乎与CHD人群的扩张并不匹配,尤其是在成人中。应进一步投资和改变政策以增加供体数量,增加CHD移植能力,以应对潜在CHD受者的增多,并优化这一不断增长人群的移植结局。
原始出处:
Konstantinos Dimopoulos. Heart or heart-lung transplantation for patients with congenital heart disease in England. Heart. 12 January 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心肺#
36
#心肺移植#
35
#ART#
34
#先天性#
26
#HEART#
29