Cell:诱导人胚胎干细胞快速和高效地产生12种高纯度的中胚层细胞群体
2016-07-17 生物谷 生物谷
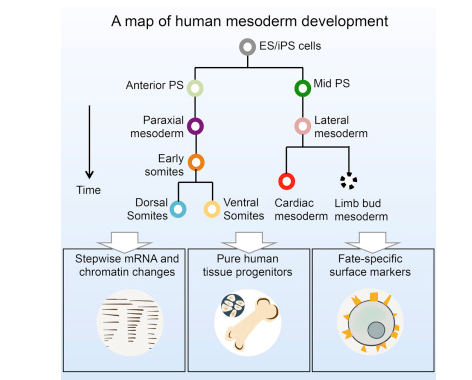
在一项新的研究中,来自美国斯坦福大学医学院的研究人员绘制出快速地和高效地指导人胚胎干细胞变成骨细胞、心肌细胞和软骨细胞等12种细胞中任何一种纯的细胞群体所必需的生物学信号和化学信号。相关研究结果发表在2016年7月14日那期Cell期刊上,论文标题为“Mapping the Pairwise Choices Leading from Pluripotency to Human Bone, He
在几天内而不是之前需要几周或几个月制造这些纯的细胞群体的能力是实现临床上有用的再生医学的关键一步---潜在地允许科学家们产生新的跳动的心脏细胞来修复心脏病发作后的损伤,或者制造软骨或骨组织让破旧的关节再次恢复新的活力或从创伤中愈合。
这项研究也强调了关键的胚胎分节(embryo segmentation)期间发生的但持续时间不长的基因表达模式,并且证实人发育似乎依赖在很多动物中进化上保守的过程。这些认识可能也有助更好地了解先天缺陷是如何发生的。
Weissman博士说,“再生医学依赖将人多能性干细胞分化为能够移植到病人体内并且发挥功能的特化组织干细胞的能力。我们花了几年时间才能够分离出造血干细胞和造脑干细胞(brain-forming stem cell, 即形成大脑的干细胞)。在这项新的研究中,我们利用我们对很多其他动物模型发育生物学的了解提供正信号因子和负信号因子来指导这些组织干细胞和器官干细胞的发育选择。在5到9天内,我们能够产生几乎所有我们需要的纯细胞群体。”
探究奥秘
胚胎干细胞是多能性的,这意味着它们能够变成体内任何一种细胞。为了做到这一点,它们对发育中的胚胎内的多种时间特异性和位置特异性的信号作出应对,从而指导它们变成特定类型的细胞。针对这种过程在鱼、小鼠和青蛙等动物中如何受到控制,科学家们已了解很多。
不同于很多其他动物的是,人胚胎发育是一个神秘的过程,特别是在受孕后的头几个星期内。这是因为在体外培育人胚胎超过14天在许多国家和科学界是被禁止的。但是科学家们确实知道像其他动物一样,最早阶段的人胚胎由三个胚层组成:外胚层、内胚层和中胚层。
当胚胎发育时,每种胚层负责产生某些类型的细胞。比如,中胚层产生关键的细胞类型,包括心肌细胞、骨骼肌细胞、结缔组织细胞、骨细胞、血管细胞、血细胞、软骨细胞、某些肾细胞和皮肤细胞。
Loh说,“产生这些纯的细胞群体的能力对任何一种临床重要的再生医学而言是非常重要的,而且有助绘制出人胚胎发育的基本路线图。在此之前,制造这些细胞需要几周到几个月的时间,这主要是因为不能够准确地控制细胞命运。其结果就是,科学家们最终获得不同类型细胞的混杂物。”
Loh和Chen想知道是什么信号驱动源自中胚层的每种细胞类型的形成。为了做到这一点,他们利用人胚胎干细胞系开展研究,随后通过化学信号诱导让它们转化为形成早期胚胎的中空细胞球表面上的原条(primitive streak)。他们接着利用已知信号分子(包括WNT、BMP和Hedgehog)的不同组合开展实验,以便诱导人胚胎干细胞变成更加特化的前体细胞。
一种既肯定又否定的策略
他们了解到人胚胎干细胞经常在众多两种可能的选择中进行一系列连续的选择,从而沿着发育途径进行发育。
最快捷和最有效的在微观上调节人胚胎干细胞发育选择的方法是促进它们分化为一种细胞类型,同时也积极地阻断它们选择另一种不同的细胞命运---一种既“肯定”又“否定”策略。
例如,原条中的细胞能够变成内胚层细胞或者两种中胚层细胞中的一种。抑制TGF-β的活性促进这些细胞选择一种中胚层细胞命运。加入一种信号分子WNT,同时阻断另一种分子BMP的活性,促进这些细胞分化为一种中胚层细胞;相反地,加入BMP,同时阻断WNT,促进这些细胞变成另一种中胚层细胞。
Loh说,“在这个过程中,我们了解到同样重要的是,要理解不想要的细胞类型是如何产生的,并且发现一种阻断这个不想要的过程,同时促进发育途径沿着我们真正想要的方向进展下去。”
通过在发育途径中的每个分叉口,仔细地指导这些细胞的选择,Loh和Chen能够让它们产生骨细胞前体细胞(bone cell precursor),而且当将这些骨细胞前体细胞移植到实验室小鼠体内时,能够形成人骨组织,此外,这些前体细胞还能产生跳动的心肌细胞和另外10种中胚层细胞系。
在每个发育阶段,研究人员进行单细胞RNA测序以便鉴定独特的基因表达模式和评估单个细胞群体的纯度。通过研究单个细胞中的基因表达谱,他们能够鉴定出之前未知的瞬时状态(transient state),这些瞬时状态是前体细胞分化为更加特化的细胞时的典型特征。
特别地,他们首次观察到在人胚胎分节后形成将发育为人体的头部、躯干和四肢的不连续部分之前出现的基因表达瞬时脉冲。这个过程反映了已知在其他动物体内发生的情形,并且证实人胚胎发育中的这个分节过程在进化上是保守的。
Loh说,“胚胎分节是人发育的一个基本步骤。如今,我们能够看到它是一个非常保守的过程。”了解分节和其他关键发育步骤何时和如何发生可能有助理解当这些步骤发生差错时,先天性出生缺陷如何产生。
快速产生纯的特化前体细胞群体的能力为进一步开展研究打开大门。
Loh说,“接下来,我们想要证实这些不同的前体细胞能够再生它们各自的组织,而且甚至可能缓解动物模型中的疾病。”
原始出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#群体#
38
#Cell#
31
#CEL#
32
更加灵敏你你你你你你公民
61
干细胞诱导一直在不断研究中!
96
#胚胎#
29
#胚胎干细胞#
42
效率非常高,技术也越来越成熟,这样你未来应用应该是不远了,尤其是能够分离出高纯度的细胞。
75