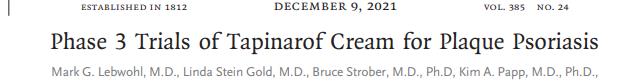
NEJM:Tapinarof乳膏局部治疗银屑病III期临床获得成功
2021-12-09 MedSci原创 MedSci原创
每日一次1%Tapinarof乳膏局部治疗可显著缓解斑块型银屑病患者症状。
银屑病是一种慢性,免疫介导的皮肤病,影响全球约2%人口。目前已有多种全身靶向和生物疗法用于成人中重度银屑病的治疗,然而局部治疗仍然是大多数银屑病患者的首选,特别是局部疾病及短期治疗中。大多数局部疗法需要使用糖皮质激素导致局部方案在使用时间、范围和应用部位方面受限。Tapinarof乳膏是一种局部芳香烃受体调节剂,可通过调节白细胞介素-17、皮肤屏障丝聚蛋白和loricrin的表达治疗银屑病。近日研究人员公布了Tapinarof乳膏III期临床研究结论。
轻度至重度斑块型银屑病患者参与研究,包含2个平行研究。患者基线PGA得分为2(轻度)至4(重度,PGA评分范围为0至4,得分越高表示银屑病症状越严重),患者受影响皮肤面积占总体表面的3%至20%,患者每天使用一次1%TAPINAR或安慰剂乳膏,持续12周。主要终点PGA治疗应答,定义为PGA评分为0(清晰)或1(几乎清晰)或第12周时较基线至少降低2分。次要疗效终点包括银屑病面积和严重程度指数(PASI)评分至少降低75%,PGA评分为0或1,受影响的体表面积百分比变化, PASI评分至少降低90%。患者报告结果包括瘙痒峰值评分(PP-NRS,0-10,得分越高瘙痒越严重)、PP-NRS总分、皮肤病生活质量指数总分和银屑病症状日得分至少下降4分。
在试验1和试验2中,分别对692和674名患者进行了筛查,其中510名和515名患者纳入研究。试验1中,Tapinarof组35.4%的患者出现PGA应答,对照组6.0%的患者出现PGA应答。试验2中,分别有40.2%和6.3%的患者出现PGA应答。次要终点的结果和患者报告的结果与主要终点趋势相同,Tapinarof治疗组占优。Tapinarof乳膏的不良反应包括毛囊炎、鼻咽炎、接触性皮炎、头痛、上呼吸道感染和瘙痒。
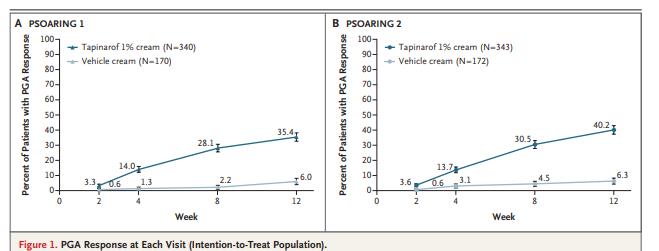
Tapinarof治疗后PGA响应率显著提高
研究认为,每日一次1%Tapinarof乳膏局部治疗可显著缓解斑块型银屑病患者症状。
原始出处:
Mark G. Lebwohl et al. Phase 3 Trials of Tapinarof Cream for Plaque Psoriasis. N Engl J Med,December 9,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#III#
42
#I期临床#
43
#局部#
40
#局部治疗#
0
#II期临床#
37
#III期#
30
好
55
非常好
62