Neurology:卒中后癫痫影响青年卒中患者长期功能预后
2013-12-03 佚名 丁香园
该研究的目的是研究青年卒中幸存者发生卒中后癫痫对长期功能预后的影响。 该研究为前瞻性队列研究,共纳入537例年龄在18到50岁间的卒中幸存者,其为首次发生的短暂性脑缺血发作、缺血性卒中和出血性卒中。在平均随访9.8年后,评价卒中后癫痫与功能预后的关系。使用logistic回归分析改良后Rankin评分(mRS评分大于2分)及日常活动评价工具评分(IADL小于8分)评价显示的不良预后优势比
该研究的目的是研究青年卒中幸存者发生卒中后癫痫对长期功能预后的影响。
该研究为前瞻性队列研究,共纳入537例年龄在18到50岁间的卒中幸存者,其为首次发生的短暂性脑缺血发作、缺血性卒中和出血性卒中。在平均随访9.8年后,评价卒中后癫痫与功能预后的关系。使用logistic回归分析改良后Rankin评分(mRS评分大于2分)及日常活动评价工具评分(IADL小于8分)评价显示的不良预后优势比。【原文下载】
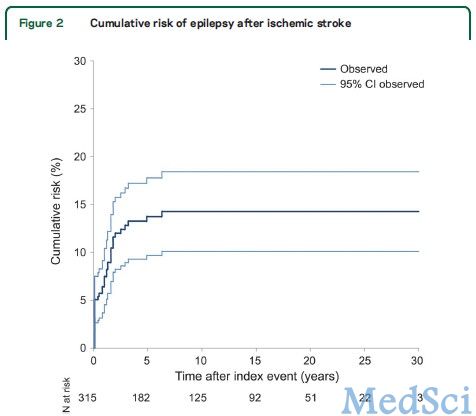
在纳入的537例青年卒中幸存者中,有40例缺血性卒中患者,4例TIA患者,10例出血性卒中患者发生卒中后癫痫。发生癫痫的缺血性卒中患者通过改良Rankin评分和IADL评价显示其功能预后较差。而在TIA患者和出血性青年卒中患者中,其功能预后没有明显差别。多元回归分析显示卒中后癫痫为缺血性卒中不良预后的独立危险因素。相反,IADL评分却没显示出有相关性。
青年卒中患者发生卒中后癫痫为一种常见的临床问题,可影响卒中患者的功能预后,甚至在缺血性卒中发生10年后对预后仍有一定影响。
研究背景:
青年卒中,即发生在18到50岁间的卒中,病因多为动脉夹层分离、心源性栓塞、非动脉粥样硬化性血管病和高凝状态,而50岁以上的成人传统的动脉粥样硬化危险因素则是其主要原因。青年处于人生的黄金时期,正确的治疗青年人脑血管病,或能在亚临床阶段,及早去发现青年人脑血管病的危险因素,研究青年卒中的预后影响因素,尤为重要。
原文出处:
Arntz RM, Maaijwee NA, Rutten-Jacobs LC, Schoonderwaldt HC, Dorresteijn LD, van Dijk EJ, de Leeuw FE.Epilepsy after TIA or stroke in young patients impairs long-term functional outcome: The FUTURE Study.Neurology. 2013 Nov 26;81(22):1907-13. doi: 10.1212/01.wnl.0000436619.25532.f3. 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#卒中患者#
39
#Neurol#
31
#卒中后#
31
#青年卒中#
38
#功能预后#
40