新证据!阿司匹林可减缓结肠癌、胰腺癌细胞扩散
2016-12-19 陈莫伊 生物探索
导语:先前的研究发现低剂量的阿司匹林能够降低某些类型胃肠道癌症的风险。但阿司匹林阻碍肿瘤生长的机制一直仍不清楚。近日,科学家们证实,阿司匹林减缓结肠癌和胰腺癌细胞扩散的作用与血小板有关。11月30日,发表在American Journal of Physiology - Cell Physiology上的一项研究中,来自俄勒冈健康与科学大学(Oregon Health and science un
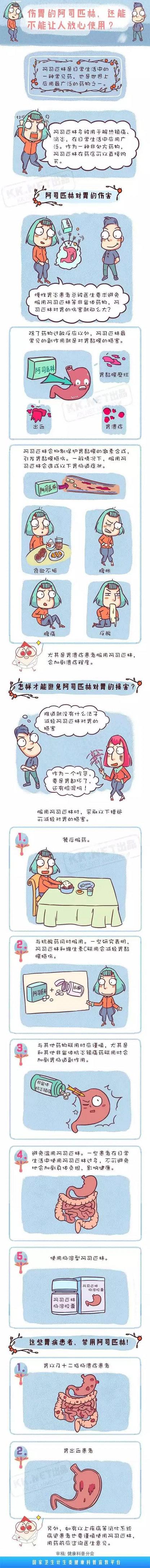
导语:先前的研究发现低剂量的阿司匹林能够降低某些类型胃肠道癌症的风险。但阿司匹林阻碍肿瘤生长的机制一直仍不清楚。近日,科学家们证实,阿司匹林减缓结肠癌和胰腺癌细胞扩散的作用与血小板有关。
11月30日,发表在American Journal of Physiology - Cell Physiology上的一项研究中,来自俄勒冈健康与科学大学(Oregon Health and science university)的研究人员发现,阿司匹林能够减缓某些类型结肠癌和胰腺癌细胞的扩散。

先前的研究发现低剂量的阿司匹林(一种抗血小板药物)能够降低某些类型胃肠道癌症的风险。但阿司匹林阻碍肿瘤生长的机制一直仍不清楚。据了解,血小板能够通过释放生长因子,以及增加调节肿瘤细胞发展的某种蛋白的响应,促进癌细胞生长。研究人员表示,这一研究的目的是为了确定阿司匹林治疗对血小板激活和功能的抑制作用。
具体来说,研究中,科学家小组将激活的血小板与3组癌细胞混合。这3组癌细胞分别是转移性结肠癌细胞、非转移性结肠癌细胞以及非转移性胰腺癌细胞。当将阿司匹林添加到混合物中,他们发现,血小板不再能够刺激胰腺癌细胞和非转移性结肠癌细胞的生长和增殖。但使用阿司匹林处理后,转移性结肠癌细胞继续增加。
研究人员表示,在胰腺癌细胞中,低剂量的阿司匹林就能够阻止血小板释放生长因子,阻碍癌蛋白信号。但只有非常高剂量的阿司匹林才能够有效阻止转移性结肠癌细胞的生长。
这一研究描述了血小板、阿司匹林和肿瘤细胞之间相互作用,有望帮助非转移性癌症的治疗。研究人员表示,这一研究揭示了高剂量和低剂量阿司匹林对不同肿瘤起源的转移性和非转移性癌细胞作用机制的重要差异和特异性。
除这一抗癌作用的新证据外,近日,发表在PLOS ONE杂志上的一项研究中,南加州大学(USC)的研究人员发现,对具有高心脏病风险的老年美国人来说,每天服用低剂量的阿司匹林能够降低心脏病发作的风险,预防某些癌症和癌症相关死亡,并延长寿命,挽救患者的生命。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌细胞扩散#
22
‘’使用阿司匹林处理后,转移性结肠癌细胞继续增加‘’。这话听着像阿司匹林促进了转移结肠癌的发展啊
65
血小板能够通过释放生长因子,以及增加调节肿瘤细胞发展的某种蛋白的响应,促进癌细胞生长。
59
#癌细胞#
33
123213123
73
学习看英文文献
58
好早以前就听说,如今变成一篇优秀的论文,思路来源于临床,最终回归临床
62
真的吗?!
22
老药新用
28