Cell:染色体碎裂带来医学奇迹
2015-02-16 佚名 生物360
这里要讲述的故事可以说是一个科学奇闻,抑或是一个医学奇迹。从前有个女孩从小患有严重的遗传学免疫疾病,但她居然在三十多岁的时候自己痊愈了。科学家们发现,她的痊愈是因为造血干细胞中发生了DNA破碎,去除了一个有害的基因。这个故事的主角生活在美国俄亥俄州的辛辛那提,她小时候总是反复遭遇细菌感染。医生发现,她体内负责抵御入侵细菌的白细胞水平异常低。1964年,《新英格兰医学》上的两份报告描述了这个女孩的病
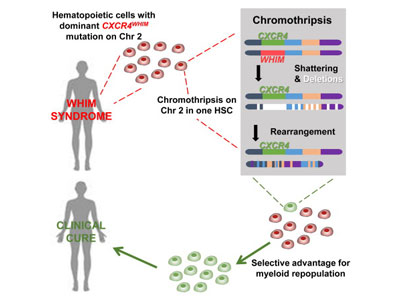
这个故事的主角生活在美国俄亥俄州的辛辛那提,她小时候总是反复遭遇细菌感染。医生发现,她体内负责抵御入侵细菌的白细胞水平异常低。1964年,《新英格兰医学》上的两份报告描述了这个女孩的病情,将其作为WHIM综合症的首个病例。这种疾病非常罕见,全世界大约只有六十名患者。这些患者能够长大成人,但是他们会因为频繁感染而出现肺部瘢痕、听觉损失和其他健康问题。而且WHIM综合症患者对可能致癌的人乳头瘤病毒高度敏感。
2003年,研究者们将CXCR4基因与WHIM关联起来。这个基因编码一种细胞表面蛋白,免疫细胞通过该蛋白来识别趋化因子。WHIM患者带有一个有缺陷的CXCR4拷贝,使得这个受体过度活化,在应该关闭的时候关不上。结果是白细胞“卡”在骨髓里无法进入血流,美国国家过敏症和传染病研究所的免疫学家Philip Murphy说。
Murphy及其同事一直在NIH临床中心研究WHIM患者,以便更好的理解这种疾病和开发抑制CXCR4的药物。两年前,一个女子带着自己的两个女儿来做检查。这名59岁的女子就是上文所述的第一位WHIM患者。她的两个二十岁的女儿遗传了这种疾病,表现出典型的WHIM症状,血细胞中也存在着CXCR4突变。然而,这位母亲自己在三十多岁以后就没有出现过严重的感染。“这让我们非常非常感兴趣,”Murphy说。
NIH开始对这位母亲进行研究,他们发现,尽管其他细胞还带有CXCR4突变,但这位女性的白细胞中已经没有CXCR4突变了。研究人员检测了这些表面上正常的白细胞,结果发现2号染色体的一个拷贝比另一个拷贝短15%。全基因组测序显示,较短的染色体拷贝曾经被打碎,缺失的那一块包含CXCR4和163个正常基因。
研究人员认为,这一现象是染色体碎裂(chromothripsis)造成的。染色体碎裂是指,一个染色体在复制过程被打碎,然后这些碎片以另一种顺序重组。染色体碎裂事件是人们四年前在一个白血病患者中发现的,偶尔也出现在其他癌症中。发生染色体碎裂的细胞一般会死亡,如果细胞存活下来就会引发癌症。
这项研究中的染色体碎裂发生在造血干细胞中,可以源源不断地为这名女性提供正常白细胞。研究人员发现,与正常CXCR4和WHIM版CXCR4相比,缺乏一个CXCR4拷贝的干细胞能够更好的移植给小鼠。正因如此,这位女性的白细胞现在全都表现正常。Murphy等人将这些研究结果发表在二月五日的Cell杂志上。
Murphy指出,这位女性身上发生的奇迹说明,染色体碎裂可以治愈疾病。以后可以在自己痊愈的罕见病患者中检测这一事件。
这一发现“非常有趣,”西奈山伊坎医学院的临床遗传学家George Diaz评论道,CXCR4突变引发WHIM就是他鉴定的。Diaz由此想到了“柏林病人”的故事,这个HIV阳性患者得了白血病,但在接受骨髓移植之后,体内就没有可检出的HIV病毒了。这是因为他的骨髓供体缺乏一种趋化因子受体,HIV需要这一受体才能进入细胞。毫无疑问,现在这项染色体破碎研究也有着重要的临床意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
28
#Cell#
31
非常好的文章,学习
135
很不错学习了
120
?学习了
120
#染色体#
24