吴一龙教授:2016年肺癌年终大盘点
2016-12-23 肿瘤资讯sophia 肿瘤资讯sophia
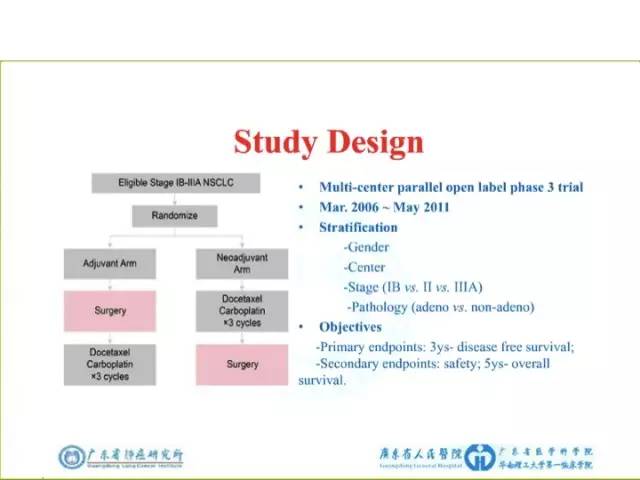
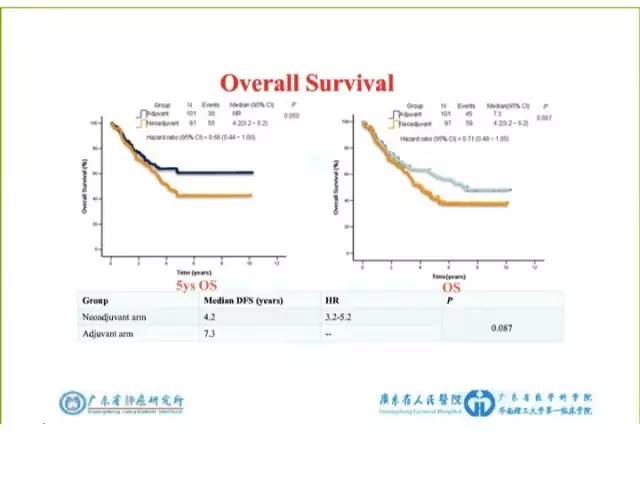
每到年末,最期待的就是吴一龙教授带来的肺癌年终大盘点,今年吴教授就“早期非小细胞肺癌,靶向治疗,EGFR TKIs耐药,脑转移,免疫治疗”五个主题展开了精彩演讲,现场气氛热烈。肿瘤资讯小编根据吴教授演讲内容进行了整理,以飨读者。 一、 早期肺癌 重点介绍了2016年ESMO大会上公布的CSLC0501(NCT00321334)研究。该项研究从2006年3月至2011
每到年末,最期待的就是吴一龙教授带来的肺癌年终大盘点,今年吴教授就“早期非小细胞肺癌,靶向治疗,EGFR TKIs耐药,脑转移,免疫治疗”五个主题展开了精彩演讲,现场气氛热烈。肿瘤资讯小编根据吴教授演讲内容进行了整理,以飨读者。


















四、脑转移 1、BRAIN研究 吴教授重点介绍了今年在WCLC上公布的BRAIN研究结果。入组标准:EGFR突变的晚期NSCLC患者存在大于3个脑转移病灶,年龄18-75岁,预期寿命大于12周,PS评分为0-1分。












小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







厉害厉害
45
受教了,多谢分享
50
好东西,收藏了
42
继续学习
54
学习了,谢谢!
54
肺癌的新进展
0
继续学习
23