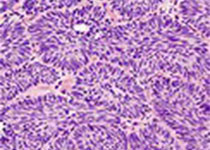
Urol J:巨噬细胞抑制因子-173基因多样性与前列腺癌生物学行为相关性研究
2018-08-30 AlexYang MedSci原创
慢性炎症是前列腺癌病因学的一个重要因子。巨噬细胞游走抑制因子(MIF)在炎症响应方面具有重要的调节作用。最近,有研究人员调查了MIF-173G/C多样性与前列腺癌发生和生物学行为之间潜在相关性。研究人员在128名前列腺癌受试者和135名对照中利用PCR-RELP技术对MIF的多样性进行了分析。研究发现,MIF-173*C等位基因的频率在前列腺癌患者(19.5%)中要比健康对照个体(10%)显著更高
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#基因多样性#
31
#相关性#
23
#多样性#
38
#抑制因子#
34
#生物学#
34
学习了,谢谢分享
66