BMC Gastroenterology:急慢性肝衰竭患者血浆超氧化物歧化酶水平与生存率的关系
2022-03-01 MedSci原创 MedSci原创
慢加急性肝衰竭(ACLF)是指各种急性损伤因素作用下,肝功能相对稳定的慢性肝病患者迅速恶化的肝衰竭综合征。
急慢性肝衰竭 (ACLF) 被定义为已患有慢性肝病的个体的肝功能急性恶化,导致多系统器官衰竭和高短期死亡率。目前,除肝移植外,尚无有效的治疗方法。ACLF 的病因因地区而异,酒精性肝病 (ALD) 和非酒精性脂肪性肝病 (NAFLD) 在美国和欧洲国家很常见,而病毒感染(尤其是 HBV 感染)在亚洲国家起主要作用。乙型肝炎病毒(HBV)表面抗原在成人中的携带率约为 8%,慢性乙型肝炎(CHB)感染是中国 ACLF 的主要原因。目前,氧化应激被认为在肝功能衰竭中起重要作用,在 ACLF 期间,受伤/死亡的肝细胞会显着增加氧化应激,从而导致额外的肝细胞损失并抑制再生,从而导致恶性循环。超氧化物歧化酶 (SOD) 通过将有毒的超氧化物转化为过氧化氢来减少 ROS 的有害影响。肝组织中的 SOD 染色显示,急性肝功能衰竭 (ALF) 患者中 SOD2 的表达增加,也称为锰依赖性 SOD (MnSOD),血浆 SOD 水平升高并与疾病严重程度相关。由于活性氧 (ROS) 在 ACLF 中起作用,因此本项研究旨在探究氧化应激的生物标志物是否有助于预测疾病的严重程度、死亡率和预后。

本项研究收集了在 2015 年 1 月至 2018 年 9 月期间存在肝脏疾病的124 名 ACLF 患者以及健康个体、肝硬化和 ALF 患者。使用 ELISA 商业试剂盒检测血浆超氧化物歧化酶 (SOD) 水平,最后使用Kaplan–Meier方法用于生存分析。
研究结果显示ACLF患者的血浆 SOD 水平在统计学上高于对照组(健康对照组和肝硬化患者);然而,该水平与 ALF 患者的水平没有差异。多变量分析以及终末期肝病模型结果显示血浆 SOD 水平可能是一种廉价、易于获得且显着的独立预后指标(HR = 1.201, 95% CI 1.001–1.403, P < 0.01)。SOD > 428 U/mL 的水平与 ACLF 患者死亡或肝移植可能性的统计学显着增加有关。血浆 SOD 水平和 MELD 评分的结合提高了测量 ACLF 患者严重程度和预后的性能。
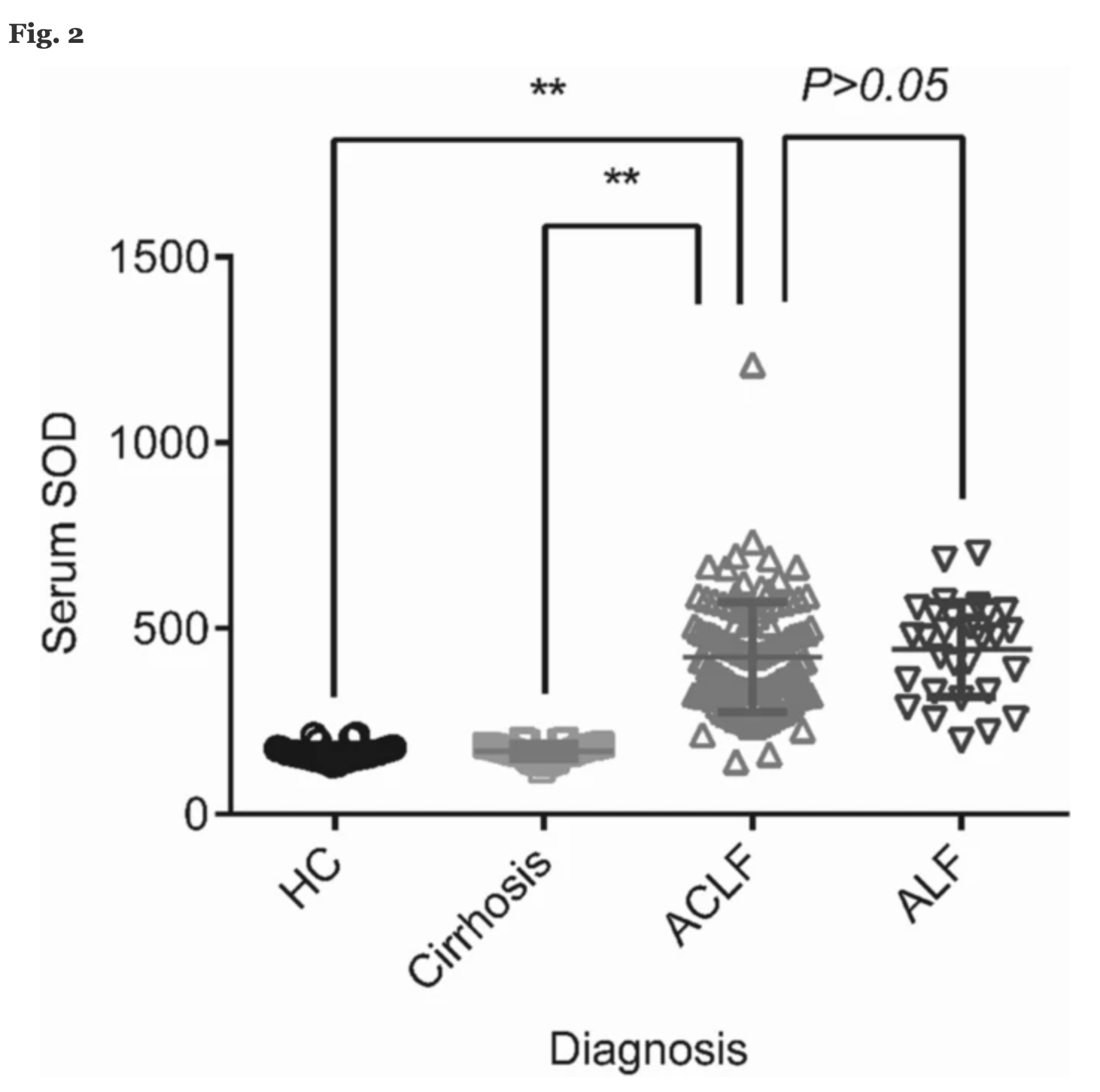
图:超氧化物歧化酶水平表达差异
本项研究证实ACLF 患者可根据入院时血浆 SOD 水平分为高危组和低危组。患者结果与 SOD 水平和 MELD 评分的组合评分高低密切相关。这种方法可用于预测患者预后并优先考虑肝移植候选者。
原始出处:
Zhen Tian. Et al. Association between plasma level of superoxide dismutase and survival of patients with acute-on-chronic liver failure. BMC Gastroenterology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AST#
48
#BMC#
43
#超氧化物#
35
#Gastroenterol#
37
#GAS#
31
这是怎么回顾性收集既往病人的血液标本的呢?
43
#肝衰#
41
#生存率#
34
#Gastroenterology#
37