目的
比较前哨淋巴结活检(SLN)与盆腔和腹主动脉旁淋巴结切除术(LND)在深浸润子宫内膜样子宫内膜癌(EEC)治疗中的肿瘤学结局;比较淋巴结阴性病例的肿瘤学结局。
方法
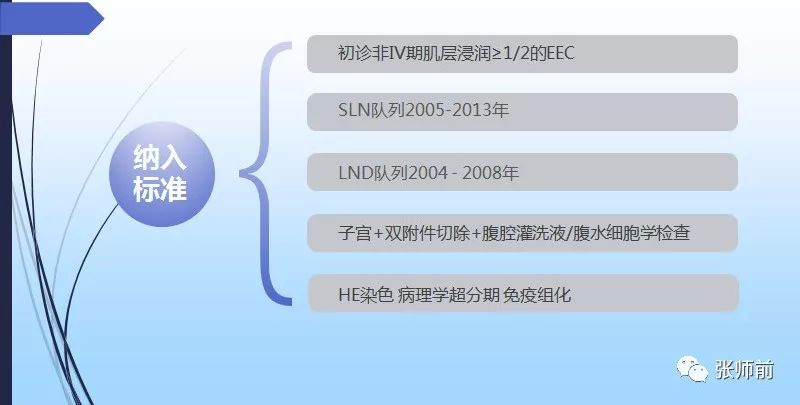
在两个机构中,确定了深浸润(≥50%子宫肌层浸润)EEC的患者。一个机构采用LND(2004-2008),另一个机构采用SLN(2005-2013)。FIGO IV期病例被排除在外。记录特征和后续数据。
结果
确定了176名患者(LND,94; SLN,82)。SLN患者更年轻(p = 0.003)并且LVSI比例更高(p <0.001)。SLN队列中9.8%和LND队列中29.8%未接受辅助治疗(p<0.001)。淋巴结评估类型与复发之间没有关联; PFS调整后的风险比(aHR; LNDvs SLN)0.87(95%CI 0.40,1.89)。在调整年龄和辅助治疗后,淋巴结评估方法与OS之间没有关联(aHR 2.54; 95%CI 0.81,7.91)。淋巴结阴性队列证明生存率和评估方法之间无关联:PFS aHR0.69(95%CI 0.23,2.03),OS 0.81(95%CI0.16,4.22)。在淋巴结阴性队列中,与无辅助治疗或仅IVRT相比,辅助EBRT +/- IVRT(HR 1.63; 95%CI 0.18,14.97)和辅助化疗+/- EBRT +/- IVRT(HR 0.49; 95%CI 0.11,2.22)均与OS无关。

结论
在深浸润EEC中采用SLN方法评估淋巴结不会影响肿瘤学结局。无论评估方法如何,在淋巴结阴性病例中存活率更高。淋巴结阴性患者的辅助化疗似乎不会影响结果。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#内膜#
51
#淋巴结#
59
#肿瘤学#
53
#前哨淋巴结#
50