BMC Med:阿帕替尼+奥沙利铂+卡培他滨新辅助治疗局部晚期胃癌/胃食管交界处癌
2022-05-02 Nebula MedSci原创
采用阿帕替尼、奥沙利铂和卡培他滨联合方案作为局部晚期胃/胃食管交界处腺癌的新辅助治疗的前期可期
胃癌是中国最常见、最致命的癌症之一。与日韩不同,中国新确诊的一半以上的胃癌患者已是晚期,即使经过正规治疗,预后也都很差。早期胃癌患者的5年总生存率高达93.6%,但晚期患者的则显著下降至17.9%。
晚期胃癌患者往往采用药物治疗。在局限性胃癌的新辅助化疗中加入抗血管生成药物被认为是一种很有前途的策略,但其临床价值尚不明确。
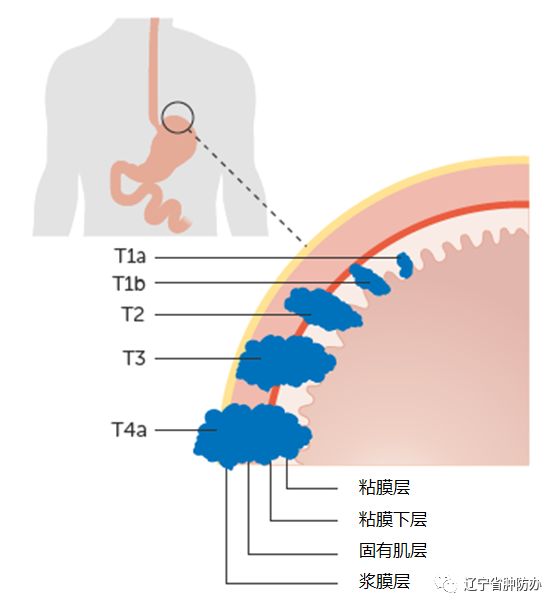
本研究是一项在上海复旦中山医院开展单中心、单臂的2期临床试验,招募了局部晚期(cT3/4aN+M0)胃或胃食管交界处(GEJ)腺癌患者,予以三个疗程的奥沙利铂(135 mg/m2,D1)、卡培他滨(1000 mg/m2,2/日,D1-14)和阿帕替尼(250 mg/日,第3个疗程剂量加倍)治疗,另加用一个疗程的奥沙利铂和卡培他滨,继以胃切除术+ D2淋巴结切除术。主要终点是客观缓解率。
无事件生存率和总生存率
2017年4月28日至2019年10月23日期间,共筛查了37位患者,其中35位被纳入研究。在32位可纳入疗效和安全性评估的患者中,客观缓解率为78.1%(25/32)。31位(96.9%)患者获得了R0切除,2位(6.3%)获得了病理完全缓解,11位(34.4%)获得了病理缓解。截止2021年9月30日,中位无事件生存期为42.6个月,中位总生存期未达到。
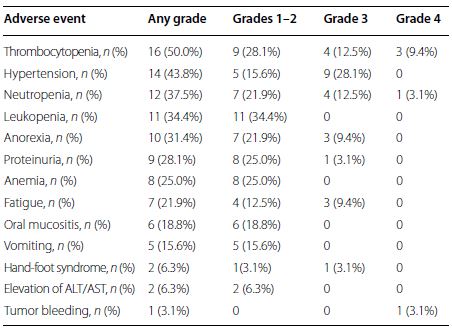
新辅助治疗期间的并发症发生情况
最常见的3/4级治疗相关不良反应事件有高血压(28.1%)、血小板减少症(21.9%)和中性粒细胞减少症(15.6%)。7位(21.9%)患者发生了手术并发症,最常见的是腹腔内脓肿(4/32, 12.5%)。
综上,采用阿帕替尼、奥沙利铂和卡培他滨联合方案作为局部晚期胃/胃食管交界处腺癌的新辅助治疗展现出可靠的疗效和可控的安全性,值得开展3期临床试验进行进一步的验证。
原始出处:
Tang Zhaoqing,Wang Yan,Yu Yiyi et al. Neoadjuvant apatinib combined with oxaliplatin and capecitabine in patients with locally advanced adenocarcinoma of stomach or gastroesophageal junction: a single-arm, open-label, phase 2 trial.[J] .BMC Med, 2022, 20: 107.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#胃食管#
60
#铂#
62
#局部晚期#
62
#新辅助#
57
#BMC#
46
#食管交界处癌#
56
#晚期胃癌#
52
#卡培他滨#
62
#局部#
38
#食管#
45