Liver Cancer:系统回顾和荟萃分析评估不可切除肝内胆管癌的放疗方式:体内或体外放疗?
2021-07-21 yd2015 MedSci原创
对于不可切除肝内胆管癌(iCCA)患者,EBRT和SIRT都是安全有效的措施。但是因为研究中较高的异质性不能很好的进行两者的比较,今后需要更高质量的研究去比较。
我们知道,对于不可切除肝内胆管癌(iCCA)患者,体外放疗(EBRT)和选择性的体内放疗(SIRT)都可选择。但是,还没有高质量的随机对照研究评估两者的疗效性。来自美国的研究团队,进行了一项系统回顾和荟萃分析,评估EBRT和SIRT在iCCA患者中的疗效。相关成果发表在Liver Cancer 杂志上。

搜索PubMed 和 Cochrane数据库2000年1月至2020年6月期间的相关文献。最终29项研究包含732例接受SIRT,以及20项研究包括443例接受EBRT的患者纳入研究分析。
根据RECIST, 调整的RECIST (mRECIST), 欧洲肝脏协会(EASL), WHO,和PERCIST标准,进行SIRT治疗患者的放疗应答(RR)分别为22% (95% CI: 10–37%), 35% (95% CI: 4–75%), 82% (95% CI: 48–100%), 24% (95% CI: 14–39%), 和 81% (95%: 63–95%)。疾病控制率(DCR)分别为75% (95% CI: 65–84%), 78% (95% CI: 64–89%), 98% (95% CI: 88–100%), 98% (95% CI: 88–100%), 和100% (95% CI: 93–100%)。进行EBRT治疗的患者, 根据RECIST, mRECIST,和EASL标准评估的RR分别为31% (95% CI: 12–54%), 46% (95% CI: 30–64),和36% (95% CI: 22–51)。DCR分别为83% (95% CI: 61–98%), 89% (95% CI: 73–96%),84% (95% CI: 71–94%)。
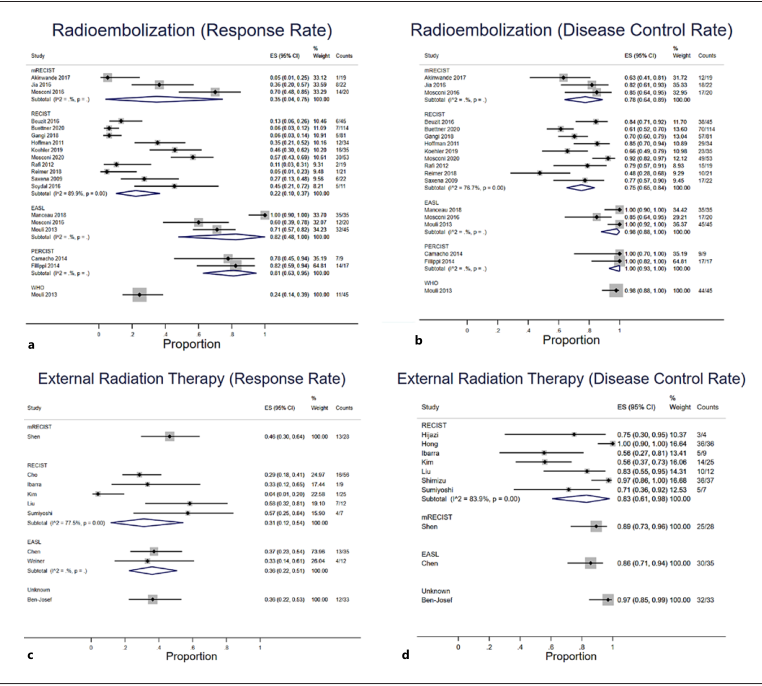
RR
SIRT治疗患者,从初始放疗开始,中位生存为12个月 (95% CI: 10.8–14.6)。6个月, 1 年, 2年, 和3 年的OS率分别为74.7% (70.3–78.5%), 52.3% (47.4–57.0%), 33.3% (28.7–37.9%),和25.3% (21.1–29.6%)。EBRT治疗患者,从初始放疗开始,中位生存为13.6个月(95% CI: 11.1–16.0)。6个月, 1 年, 2年, 和3 年的OS率分别为76.2% (70.7–80.8%), 49.8% (43.8–55.6%), 23.4%(18.6–28.6%),和9.5% (6.4–13.4%)。
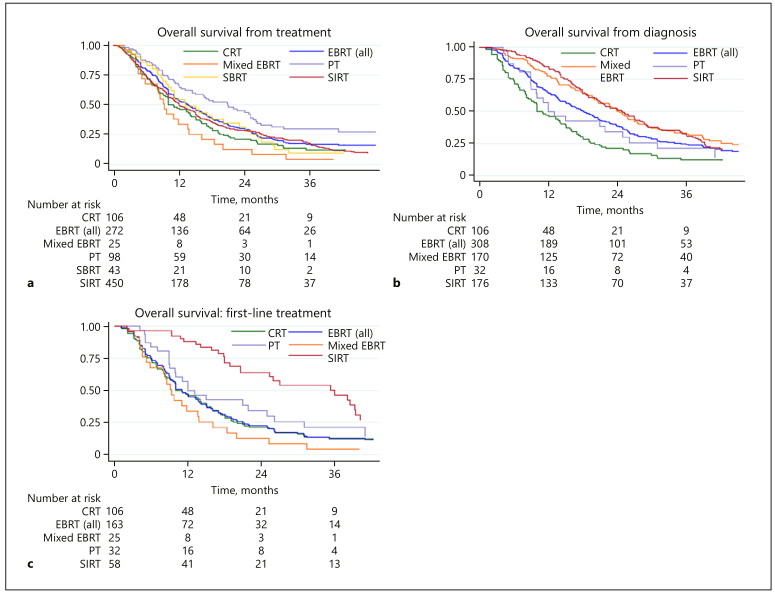
生存分析
作为一线治疗时,SIRT和EBRT的中位生存分别为36.1个月(95% CI: 20.6–39.5) 和11.0个月 (95% CI: 9.3–13.6)。SIRT治疗的6个月, 1 年, 2年, 和3 年的OS率分别为96.4% (95% CI: 86.2–99.1%), 88.6% (95% CI:76.3–94.7%), 66.3% (95% CI: 51.0–77.8%), 和56.0%(95% CI: 40.5–69.0)。EBRT治疗的6个月, 1 年, 2年, 和3 年的OS率分别为74.7%(95% CI: 67.3–80.7%), 47.0% (95% CI: 39.2–54.5%),23.3% (95% CI: 17.0–30.1%), 和13.7% (95% CI: 8.9–19.6%)。
SIRT和EBRT治疗能使患者降期手术比例分别为30.5%和18.3%。

降期后的生存
相对于SIRT,EBRT治疗出现较高几率的并发症主要有消化性溃疡(1 vs. 0.5%)、恶心(1.6 vs. 0.7%)、厌食(6.0% vs. 0)、腹痛(6.9 vs. 2.2%)、血小板减少(7.3 vs. 6.0%)、低白蛋白血症(13.2 vs. 3.3%)以及肝酶ALP (1.6 vs. 0.8%)、ALT (2% vs. 0)和胆红素(5.2 vs. 2.1%)升高。而SIRT治疗引起较高几率的并发症有贫血(7.5 vs. 0.6%),中性粒细胞减少(11.0 vs. 6.5%),以及AST升高(1.0% vs. 0.7)。
综上,对于不可切除肝内胆管癌(iCCA)患者,EBRT和SIRT都是安全有效的措施。但是因为研究中较高的异质性不能很好的进行两者的比较,今后需要更高质量的研究去比较。
原始出处:
Qian Yu,Chenyu Liu,Anjana Pillai, et al. Twenty Years of Radiation Therapy of Unresectable Intrahepatic Cholangiocarinoma: Internal or External? A Systematic Review and Meta-Analysis. Liver Cancer. DOI: 10.1159/000516880. Published online: July 19, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#荟萃#
43
#荟萃分析#
38
#肝内胆管癌#
50
#系统回顾#
47
#胆管#
44