AAC:张云等新型肽类抗生素保护临床耐药菌感染药效学研究获进展
2012-04-20 中科院昆明动物所 中科院昆明动物所
近日,美国著名药理学和药学杂志Antimicrobial Agents and Chemotherapy在线刊登了中科院昆明动物所研究人员的最新研究成果“Efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in mouse models ,”,文章中,研究者揭示了他们在新型肽类抗生素体
近日,美国著名药理学和药学杂志Antimicrobial Agents and Chemotherapy在线刊登了中科院昆明动物所研究人员的最新研究成果“Efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in mouse models ,”,文章中,研究者揭示了他们在新型肽类抗生素体内保护临床耐药菌感染药效学上的重要进展。
感染是目前医院住院病人死亡的主要原因之一,据美国新英格兰医学杂志统计,仅在美国,每年败血症的发病率为75万人,其中死亡22.5万。抗生素市场总额大约在300亿美元左右,半个世纪以来没有开发出真正意义上的新类型抗生素(Science 2009, 325, 1089)。随着传统抗生素的大量使用和滥用,在临床上出现了各种各样的耐药菌株,如携带NDM-1质粒的“超级细菌”,耐甲氧西林,万古霉素致病菌等,目前临床使用的抗生素对这些耐药菌已无疗效,成为目前特别是今后危害人类健康的重大威胁。
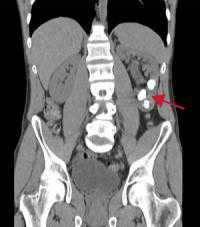
在与致病菌变异竞争的过程中,自然界各种来源的抗菌肽目前成为人们研发新型抗感染药物的希望,但毒性和低下的体内药效成为限制大多数抗菌肽用于临床药物研发的瓶颈。中国科学院昆明动物研究所动物模型与人类疾病机理重点实验室生物毒素与人类疾病课题组在张云研究员和李文辉研究员带领下,在前期大量抗菌肽研究工作和相关发明专利“爬行动物cathelicidin抗菌肽及衍生物及其应用”(专利号:ZL 2008 1 0058260.9)基础上,该课题组李盛安博士生等建立了临床耐药菌感染动物模型,深入开展了眼镜王蛇毒OH-CATH30抗菌肽及衍生物的体内药效学评价,结果表明在目前临床广泛使用的抗生素药物头孢哌酮钠无效的情况下,OH-CATH30及衍生物在安全剂量范围内(低于毒性剂量10倍以上),对于全身性和致死性耐药菌感染具有良好的治疗和保护作用,为新型抗耐药微生物感染药物的制备和临床应用提供了坚实的体内药效学基础。
该研究获得国家重大新药创制专项,国家973计划项目以及国家基金委-云南省联合基金项目的资助。

doi:10.1128/AAC.06304-11
PMC:
PMID:
Efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in mouse models
Sheng-An Lia,b, Wen-Hui Leea,* and Yun Zhanga,*
Antimicrobial peptides (AMPs) have been considered as alternatives to conventional antibiotics for drug-resistant bacterial infections. However, their comparatively high toxicity toward eukaryotic cells and poor efficacy in vivo hamper their clinical application. OH-CATH30, a novel cathelicidin peptide deduced from the king cobra, possesses potent antibacterial activity in vitro. The objective of this study is to evaluate the efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in vivo. The minimal inhibitory concentrations (MICs) of OH-CATH30 and OH-CM6 ranged from 1.56 to 12.5 μg/ml against drug-resistant clinical isolates of several pathogenic species, including Escherichia coli, Pseudomonas aeruginosa, and methicillin-resistant Staphylococcus aureus. The MICs of OH-CATH30 and OH-CM6 were slightly altered in the presence of 25% human serum. OH-CATH30 and OH-CM6 killed E. coli quickly (within 60 min) by disrupting the bacterial cytoplasmic membrane. Importantly, the 50% lethal dose (LD50) of OH-CATH30 and OH-CM6 in mice following intraperitoneal (i.p.) injection was 120 mg/kg and 100 mg/kg, respectively, and no death was observed at any dose up to 160 mg/kg following subcutaneous (s.c.) injection. Moreover, 10 mg/kg OH-CATH30 or OH-CM6 significantly decreased the bacterial counts as well as the inflammatory response in a mouse thigh infection model and rescued infected mice in a bacteremia model induced by drug-resistant E. coli. Taken together, our findings demonstrate that the natural cathelicidin peptide, OH-CATH30, and its analogs exhibit relatively low toxicity and potent efficacy in mouse models, indicating that they may have therapeutic potential against the systemic infections caused by drug-resistant bacteria.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#药效学#
47
#药效#
35
#药效学研究#
31
#耐药菌感染#
27
#研究获进展#
0
#耐药菌#
31