Front Oncol:腹腔镜全胃切除术(LTG)和腹腔镜全胃切除术(LTG)治疗晚期胃癌的疗效
2021-12-14 yd2015 MedSci原创
研究表明,腹腔镜全胃切除术(LTG)非劣效于腹腔镜全胃切除术(LTG),但建议在有丰富经验的中心进行。
鉴于腹腔镜全胃切除术(LTG)的技术难度和操作复杂性,与开放全胃切除术(OTG)相比,LTG在晚期胃癌(AGC)领域的技术和肿瘤安全性尚不确定。因此,来自国内学者联合开展了回顾性倾向性评分匹配(PSM)研究,比较LTG和OTG在AGC患者中的疗效。相关结果发表在Frontiers in Oncology杂志上。
该研究为多中心研究,在2011年1月1日至2015年12月31日期间,来自3个中心的588例患者接受了首次全胃切除和D2淋巴结清扫手术,由训练有素、经验丰富的外科医生进行,并且病理证实的局部AGC (T2N0-3、T3N0-3或T4N0-3)。他们的临床数据是从三个参与中心收集的。经1:1倾向评分匹配(PSM)后,450例(LTG, n = 225;OTG, n = 225)均符合条件并进行评估。
与OTG治疗相比,LTG组的估计失血量显著降低(120 vs 200 ml, p<0.001),近端切除缘长度较长(3 vs. 2 cm, p <0.001),术后住院时间显著缩短(11 vs 13天,p<0.001)。然而,LTG的手术时间明显延长(262 vs 180 min, p<0.001)。两组在近端和远端切缘状态、淋巴结切除数目等等方面无明显差异。同样,两组均达到最少淋巴结活检数目(95.6% vs. 96.0%, p > 0.999)。
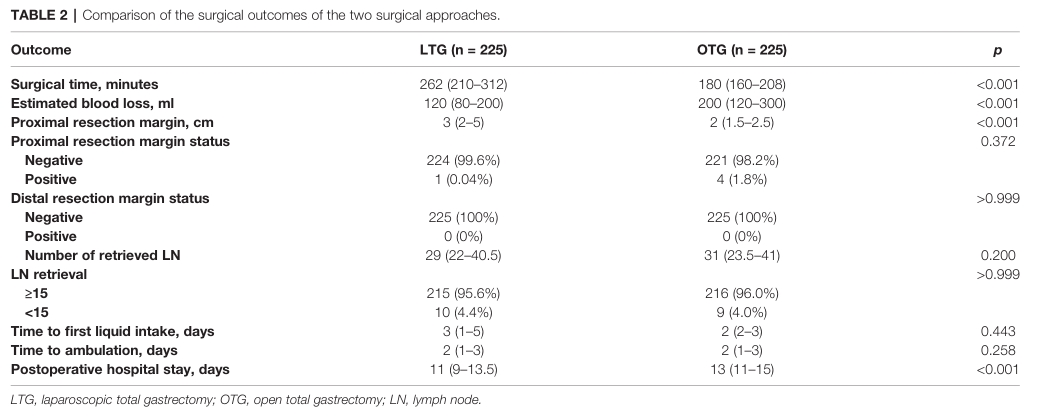
两组的手术结果
LTG与OTG在死亡率上无显著差异(RR 0.000,95%CI 0.000-3.828,p>0.999)。与OTG相比,LTG整体明显减少术后并发症(RR 0.583,95%CI 0.353 - 0.960,p = 0.047),减少内部腹部脓肿的发病率(RR 0.318,95%CI 0.141 - 0.710,p = 0.006)。
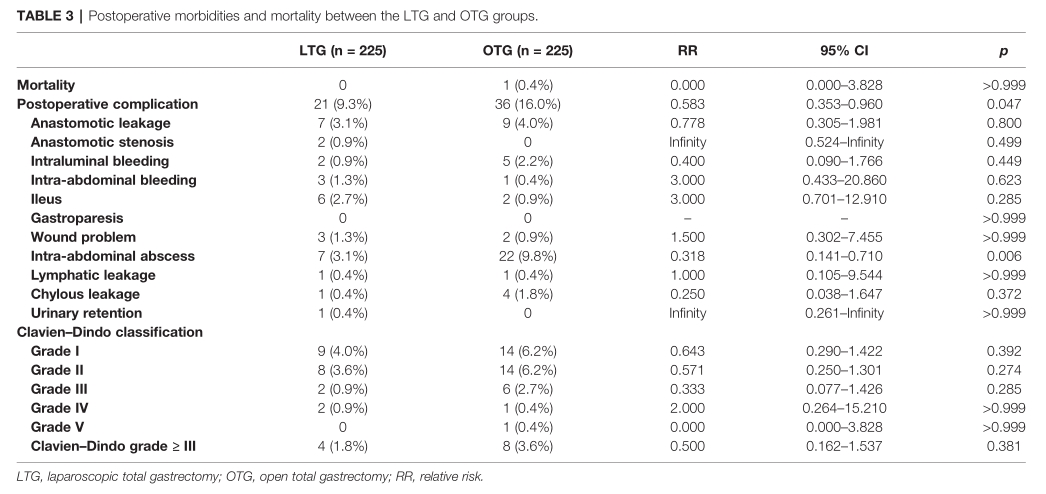
两组的并发症
中位随访期为58个月(范围为2-90个月)后,LTG和OTG治疗的5年DFS和OS率相似(5年DFS: 48.0% vs. 50.6%, p = 0.122;5年OS:48.9% vs. 51.1%, p = 0.134 2)。
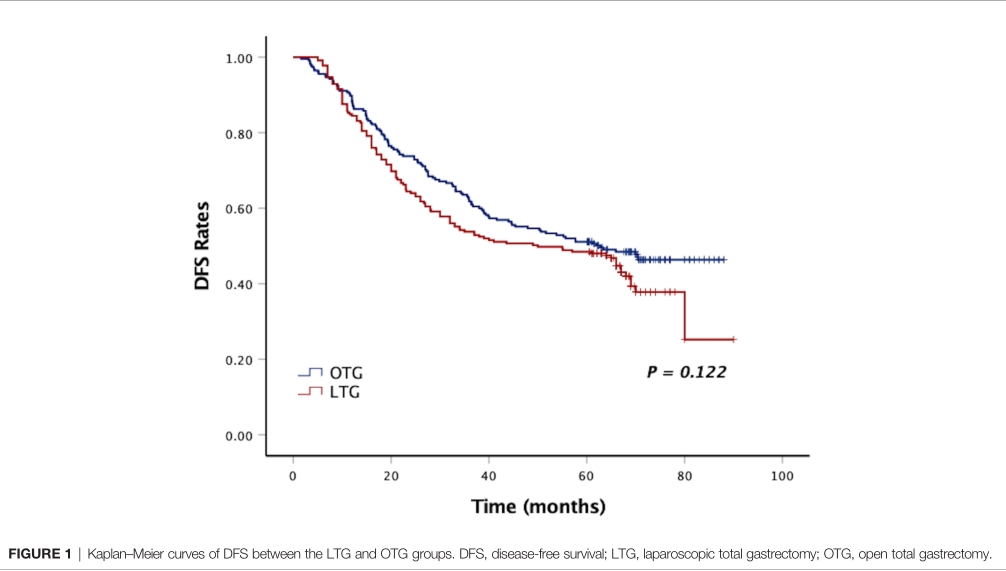
DFS
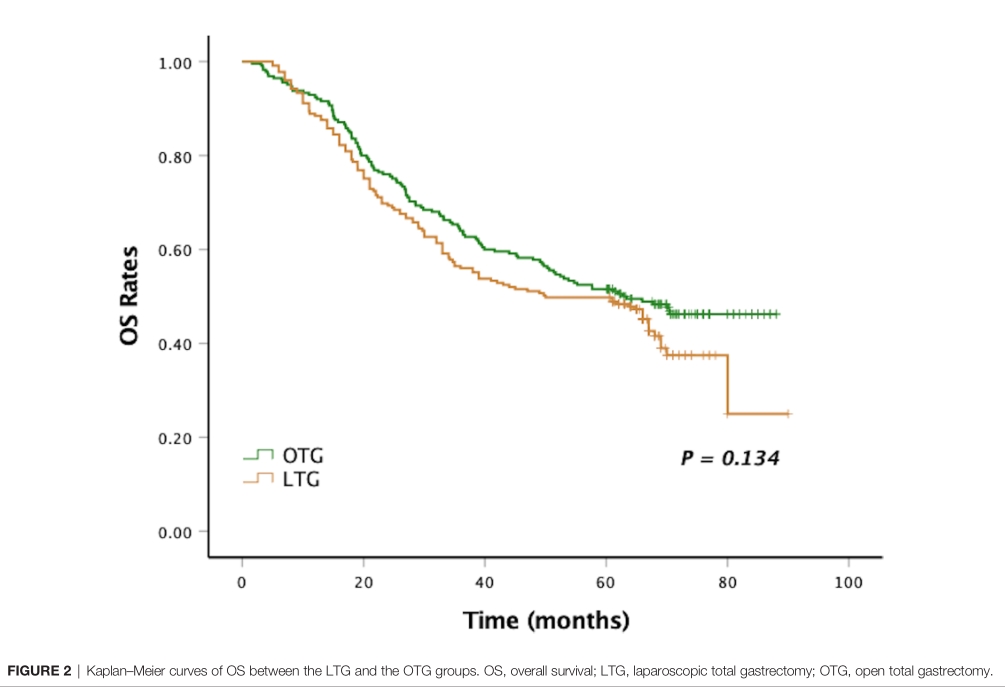
OS
单因素分析显示,肿瘤大小、肿瘤组织学、转移淋巴结数量、pT分期、pN分期和pTNM分期与DFS和OS相关。多因素分析确定pT期和pTNM期为DFS和OS的独立预后因素。手术技术未能成为DFS或OS的独立危险因素(HR 1.218, 95% CI 0.948-1.565, p = 0.123;HR 1.211, 95% CI 0.942-1.556, p = 0.135)。
综上,研究表明,腹腔镜全胃切除术(LTG)非劣效于腹腔镜全胃切除术(LTG),但建议在有丰富经验的中心进行。
原始出处:
Feng X, Chen X, Ye Z, Xiong W, Yao X, Wang W, Wang J, Chen L and Li Y (2021) Laparoscopic Versus Open Total Gastrectomy for Advanced Gastric Cancer: A Multicenter, Propensity Score-Matched Cohort Study in China. Front. Oncol. 11:780398. doi: 10.3389/fonc.2021.780398
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
21
#Oncol#
29
#腹腔镜#
45
#晚期胃癌#
34
#胃切除#
34