突破7个难点,做RT-PCR达人
2016-03-17 子非鱼 解螺旋
在初遇Real time PCR时,就听说这是个实验黑洞,大部分实验菜鸟都会深陷其中,无法自拔。小鱼也曾在Real time PCR这个坑里跌爬滚打了很长时候,同时也积累不少经验。现在就跟大家分享下我做Real time PCR的一些心得吧。 正所谓知彼知己,方能百战百胜。首先我们要先了解下Real time PCR的基础知识。 Real time PCR做为常规PCR的衍生反应,主要
在初遇Real time PCR时,就听说这是个实验黑洞,大部分实验菜鸟都会深陷其中,无法自拔。小鱼也曾在Real time PCR这个坑里跌爬滚打了很长时候,同时也积累不少经验。现在就跟大家分享下我做Real time PCR的一些心得吧。
正所谓知彼知己,方能百战百胜。首先我们要先了解下Real time PCR的基础知识。
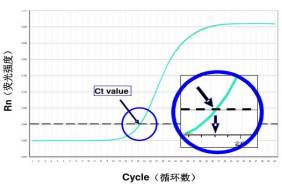
Real time PCR做为常规PCR的衍生反应,主要是通过荧光信号的变化实时监测PCR扩增反应中每一个循环扩增产物量的变化,通过ct值和标准曲线的关系对起始模板进行定量分析。
RT-PCR的具体数据就是基线(baseline),荧光阈值(threshold)和Ct值。 第 3-15 个循环的荧光值就是基线(baseline),是由于测量的偶然误差引起的。阈值(threshold)是指在扩增曲线的指数增长区域内的适当位置上设定的荧光检出界限,一般是基线的标准偏差的 10 倍。Ct 值就是每个反应管里的荧光值达到阈值时的 PCR 循环次数。Ct 值跟初始模板的量成反比。


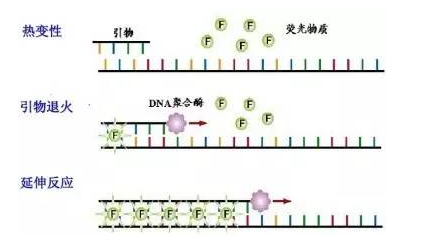
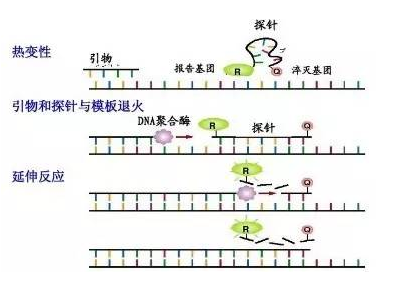
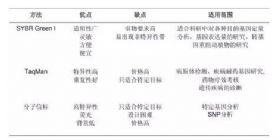
Real time PCR 的标记方法一般包括以下几类:荧光染料嵌合法(SYBR Green I)和荧光探针法(Taqman探针)和分子信标法。
SYBR Green I 法
Taqman探针法
分子信标法

三种荧光定量PCR方法的应用比较
荧光定量PCR的主要应用
原理清楚了,接下来就是实验操作及数据分析了。就在这一步,RT-PCR准备了很多大坑静待我们跳进去。难怪之前的学长要告诉小鱼,这个实验做多了,很有可能会成为思想家。果不其然,小鱼在这个实验上失败了N多次且寻觅原因无果后,便开启了哲学模式,一开口就是些人生感悟,满满的沧桑感。
那么RT-PCR究竟难在哪里呢?又该怎么处理呢?




一般,DNA样品的定量标准品为基因组DNA&质粒,RNA样品的定量标准品为Total RNA&cDNA&体外转录RNA。绘制标准曲线的标准品梯度的选择一般为5~6个梯度,标准品的稀释倍数通常为10。


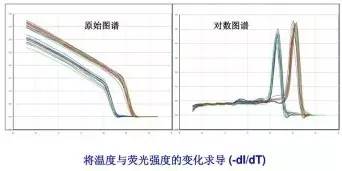
SYBR Green I 法进行检测时,可根据熔解曲线确认PCR产物的特异性。曲线横坐标是温度,纵坐标是荧光强度的变化值(不是强度本身)。其原理是依据温度从60度升至90度时,荧光强度的变化值。当温度达到PCR产物的Tm(双链DNA分子解链一半时的温度)时,荧光强度变化最大(峰值)。

绝对定量中,LOG(起始浓度)与循环数呈线性关系,通过已知起始拷贝数的标准品可制作出标准曲线,即得到该扩增反应存在的线性关系。然后根据样品的Ct值,来确定未知样品的初始模板拷贝数或浓度。通常用于病毒、细菌、衣原体、支原体的定量检测及转基因食品的检测。
相对定量用于测定单个样品基因的差异表达分析或者比较两个或两个以上样品中某个基因表达量的变化,则其结果必须用内对照基因(管家基因)校正。管家基因通常指维持细胞基本代谢活动所必须的基因,如GAPDH/Actin/18s rRNA等,实际操作中可依据文献或具体实验进行筛选。相对定量的分析方法主要有两种:双标准曲线法和2^-△△Ct法。
双标准曲线法:
每次实验都要分别用标准品做内参基因和目的基因的标准曲线,并同时扩增各待测样本中的目的基因和内参基因。然后使用标准曲线来计算待测样本中的目的基因和内参基因的表达量。最后通过公式就可以计算出目的基因的表达差异了。

2^-△△Ct法
这是最常用的进行相对基因表达分析的方法,得到的结果是实验组中目的基因相对于对照组中目的基因表达的差异倍数。要求目的基因和内参基因的扩增效率相同,且相对偏差不超过 5%。

若是目的基因和内参基因的扩增效率不一样时,可以套用以下公式来计算基因表达的差异。

其中,E1:目的基因引物扩增效率;E2:内参基因引物扩增效率;△Ct1:实验组目的基因Ct值差;△Ct2:对照组目的基因Ct值差。(E1=E2=1时,该公式=2^-△△Ct)。
如此下来,小伙伴是否觉得Real-time PCR并没有想象中那么难呢?那就快快行动起来,一举把该实验拿下吧!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#RT-PCR#
0
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
53
以前做过,好久了
94
好多东西都不明白了
88
#PCR#
21
好,谢谢
153