PloS ONE:RASSF1A启动区甲基化在乳腺癌患者预后中的作用
2012-05-29 生物谷 生物谷
近日,国际著名杂志PloS ONE在线刊登了江苏省姜堰市人民医院的研究人员的最新研究成果: "The prognostic role of RASSF1A promoter methylation in breast cancer: a meta-analysis of published data"。 文章中,研究者荟萃分析后发现:RASSF1A启动子区高甲基化的乳腺癌患者无论在"无进展生存期
近日,国际著名杂志PloS ONE在线刊登了江苏省姜堰市人民医院的研究人员的最新研究成果: "The prognostic role of RASSF1A promoter methylation in breast cancer: a meta-analysis of published data"。
文章中,研究者荟萃分析后发现:RASSF1A启动子区高甲基化的乳腺癌患者无论在"无进展生存期"(DFS) 还是"总生存时间"(OS)上均有显著性统计学意义,因此,RASSF1A甲基化的检测是很有价值的临床指标,可以作为预后的独立的危险因素,值得进一步深入研究和关注。
乳腺癌的患者预后差别较大,通常以"肿瘤大小、肿瘤TNM分期、病理分级、激素受体表达"等指标来预测患者的预后,根据患者的肿瘤生物学特点选择相应的治疗,然而这些指标预测患者的预后力度还不够,不能够针对个体患者进行分层。使得预后差的患者及时接受治疗,预后良好的患者避免接受不必要的治疗,从而避免不恰当治疗带来的毒副反应。
乳腺癌的发生发展与癌基因的激活和抑癌基因的失活密切相关。大量研究发现,抑癌基因的失活与其启动子区甲基化密切相关。RASSF1A是其中一个重要的抑癌基因。它的启动子区过度甲基化后可使它的活性下降,从而影响抑癌作用,因此影响乳腺癌的发生、发展。在这篇文章中,研究人员荟萃分析了来自8个国家总样本量达到1795例的乳腺癌患者资料,统计发现:过度甲基化的RASSF1A无论在"无进展生存期"(DFS) 还是"总生存时间"(OS)上均有显著性统计学意义,所以RASSF1A甲基化可以作为乳腺癌预后的一项独立危险因素。
来自姜堰市人民医院的崔林为这篇文章的通讯作者。姜勇是该文章的第一作者。陈文德、申仕海、丁立东为该文的共同作者。来自美国俄亥俄州立大学的著名学者Amanda Ewart Toland教授为本文审稿,并做同行评议。(生物谷Bioon.com)

doi:10.1371/journal.pone.0036780
The Prognostic Role of RASSF1A Promoter Methylation in Breast Cancer: A Meta-Analysis of Published Data
Yong Jiang1, Lin Cui1*, Wen-de Chen2, Shi-hai Shen2, Li-dong Ding2
Purpose
Epigenetic alterations have been investigated as prognostic indicators in breast cancer but their translation into clinical practice has been impeded by a lack of appropriate validation. We present the results of a meta-analysis of the associations between RASSF1A promoter methylation status and both disease free survival (DFS) and overall survival (OS) in female breast cancer.
Methods
Eligible studies were identified through searching the PubMed, Web of Science and Embase databases. Studies were pooled and summary hazard ratios (HR) with corresponding confidence intervals (CIs) were calculated. Funnel plots were also carried out to evaluate publication bias.
Results
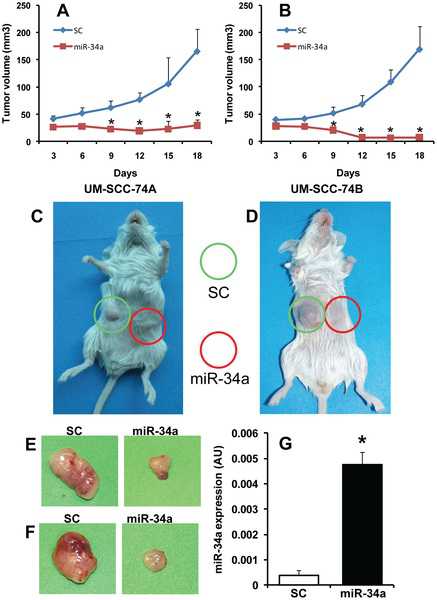
A total of 1795 patients from eight studies were included in the meta-analysis. There are eight studies which investigated DFS in 1795 cases. The relative hazard estimates ranged from 1.77–5.64 with a combined HR of 2.75 (95%CI 1.96–3.84). The HR of RASSF1A promoter methylation on DFS adjusted for other potential prognostic factors was 2.54 (95%CI 1.77–3.66). There has been five trials which analyzed the associations of RASSF1A promoter methylation status with OS in 1439 patients. The hazard estimates ranged from 1.21–6.90 with a combined random-effects estimates of 3.47 (95%CI 1.44–8.34). OS reported in multivariate analysis was evaluated in four series comprising 1346 cases and the summarized random-effects HR estimate was 3.35 (95%CI 1.14–9.85). Additionally, no publication bias was detected for both OS and DFS.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Plos one#
24
#患者预后#
27
#RASSF1A#
44
#乳腺癌患者#
29