英国医生采用基因编辑CART细胞成功治愈1岁急性淋巴细胞白血病婴儿
2015-11-07 佚名 中国新闻网
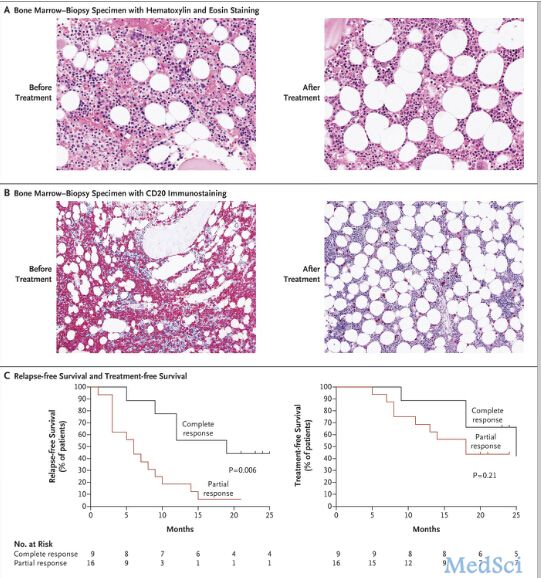
资料图片:女婴理查德兹在14周大时,确诊患急性淋巴细胞血癌。据外媒报道,英国医学界在对抗血癌方面取得重大进展,全球首次为一名一岁女婴注入经基因改造免疫细胞,成功消灭她体内的癌细胞,目前女婴已病愈回家。医生表示,女婴的病情十分严重,此次能奇迹痊愈,为运用新基因工程科技奠定里程碑,但该女婴仍需再等一、两年才能确定会否复发。医院计划展开临床测试,在其他癌童身上测试新疗法。 据报道,女婴理查

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#淋巴细胞白血病#
31
进步
89
#淋巴细胞#
35
#ART#
32
#cART#
31
肿瘤科确实大有可为
133
好厉害?
125
好厉害
96
很厉害,希望能继续研究,
101
博大精深
78