JAMA Cardiol:主动脉瓣置换术后早期LVEF改善与患者长期预后的相关性
2022-08-03 MedSci原创 MedSci原创
主动脉瓣置换术后早期LVEF改善与重度主动脉瓣狭窄患者的5年全因死亡率和心源性死亡率更低相关
在左心室射血分数(LVEF)<50%的重度主动脉瓣狭窄的患者中,经导管主动脉瓣置换术(TAVR)后早期LVEF改善与1年死亡率改善相关;但是,其与患者长期临床预后的相关性尚不明确。
该研究旨在评估TAVR后早期LVEF改善预5年预后的相关性。
该队列研究分析了PARTNER 1、2和S3试验于2007年-2015年期间招募的患者。接受经股动脉TAVR治疗的基线LVEF<50%的中高风险患者被纳入本次分析。早期LVEF改善定义:第30天时LVEF提高≥10%。主要终点是5年时的全因死亡率。
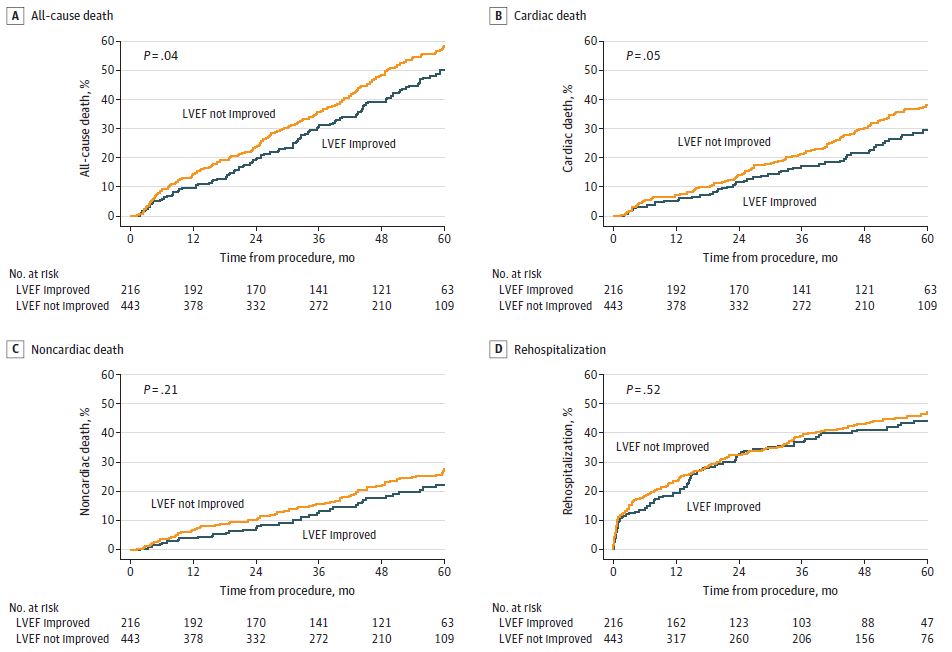
LVEF有无改善患者的生存预后
共纳入了659位基线LVEF<50%的患者,468位(71.0%)是男性,平均年龄82.4岁。216位(32.8%)患者TAVR后30天时LVEF获得改善(平均△LVEF 16.4%)。既往心肌梗死、糖尿病、癌症、基线LVEF较高、左室舒张末期内径较大和主动脉瓣面积较大均与更低的LVEF改善可能性独立相关。
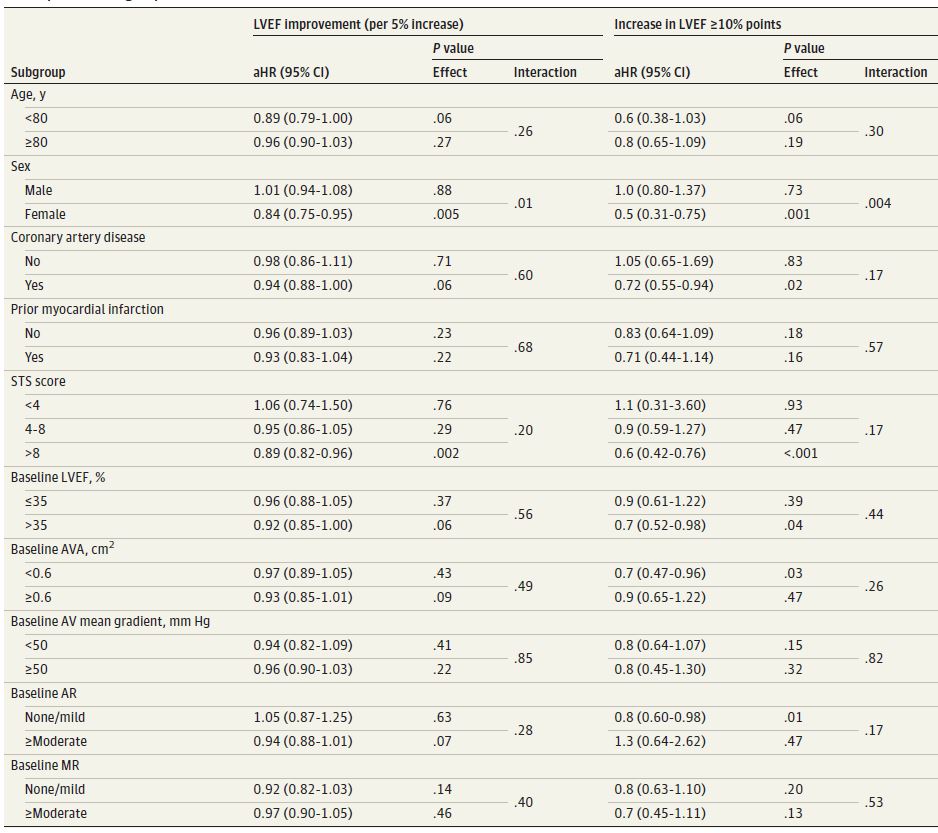
LVEF改善对患者生存预后影响的亚组分析
TAVR后LVEF改善的患者的5年全因死亡率低于无LVEF改善患者(50.0% vs 58.4%,p=0.04),心源性死亡率也相对较低(29.5% vs 38.1%,p=0.05)。在多变量分析中,TAVR后早期LVEF改善预更低的5年死亡率和心源性死亡率相关(LVEF每提高5%的校正风险比分别是0.94[p=0.04]和0.90[p=0.02])。
限制性三次样条分析显示了一个目视拐点ΔLVEF(10%),超过该拐点后,随着LVEF改善程度的增加,全因死亡率急剧下降。两组的再住院率方面无显著差异。
总之,约三分之一的LVEF<50%的重度主动脉瓣狭窄患者可在TAVR后1个月内获得LVEF改善。早期LVEF改善与5年全因死亡率和心源性死亡率更低相关。
原始出处:
Kolte D, Bhardwaj B, Lu M, et al. Association Between Early Left Ventricular Ejection Fraction Improvement After Transcatheter Aortic Valve Replacement and 5-Year Clinical Outcomes. JAMA Cardiol. Published online July 27, 2022. doi:10.1001/jamacardio.2022.2222.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#置换#
51
#Cardiol#
48
#长期预后#
38
#相关性#
33
#主动脉瓣#
36
#主动脉瓣置换术#
56
#主动脉#
43
#LVEF#
43
#置换术#
38
JAMA上文章都是顶级的,谢谢梅斯及时上新
19