J Renal Nutr:生物补充制剂对CKD患者究竟有益处吗?一项随机对照试验的荟萃分析
2022-01-08 MedSci原创 MedSci原创
研究结果强调了生物制剂对 CKD 患者的肌酐、氧化应激(丙二醛、总抗氧化能力)、炎症(白细胞介素 6)和尿毒症毒素(对甲酚硫酸盐)的标志物的有利影响。
肠道菌群失调是慢性肾病(CKD)患者的特征。尽管有研究已经提出生物补充剂可以减轻CKD患者肠道炎症和氧化应激,从而降低进行性肾损伤和心血管疾病的风险,但其效果仍然存在争议。本研究进行了一项荟萃分析,以评估生物补充制剂在 CKD 中的治疗益处。

研究者系统搜索了PubMed、Embase和Cochrane数据库中的随机对照试验,这些试验评估了 CKD(CKD3-4期至终末期肾病)患者的任何生物补充剂(益生元、益生菌、合生元)。主要结局包括肾功能、炎症标志物和氧化应激的变化。次要结局包括尿毒症毒素水平的变化和脂质代谢的变化。
842 名参与者进行了23 项符合条件的研究。研究数据表示,尽管益生元减少血清肌酸酐和血尿素氮水平,但是肾小球滤过率或血清白蛋白没有得到明显改善。生物制剂提高了总抗氧化能力和丙二醛水平,并降低了炎症标志物白介素-6,但未降低C反应蛋白。
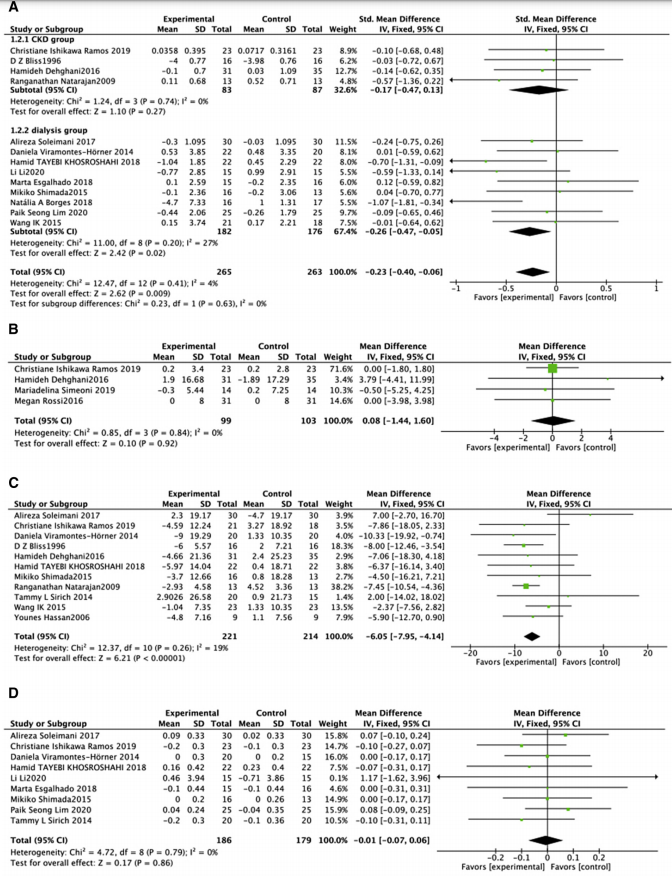
生物干预对肾功能的影响
生物干预减少了一些尿毒症毒素,包括对甲酚硫酸盐和硫酸吲哚酚,这在依赖透析的患者中有所减少。另一种毒素吲哚-3-乙酸没有变化。另外研究还发现脂质不受生物干预的影响(包括总胆固醇,高密度脂蛋白,低密度脂蛋白,甘油三酯)。
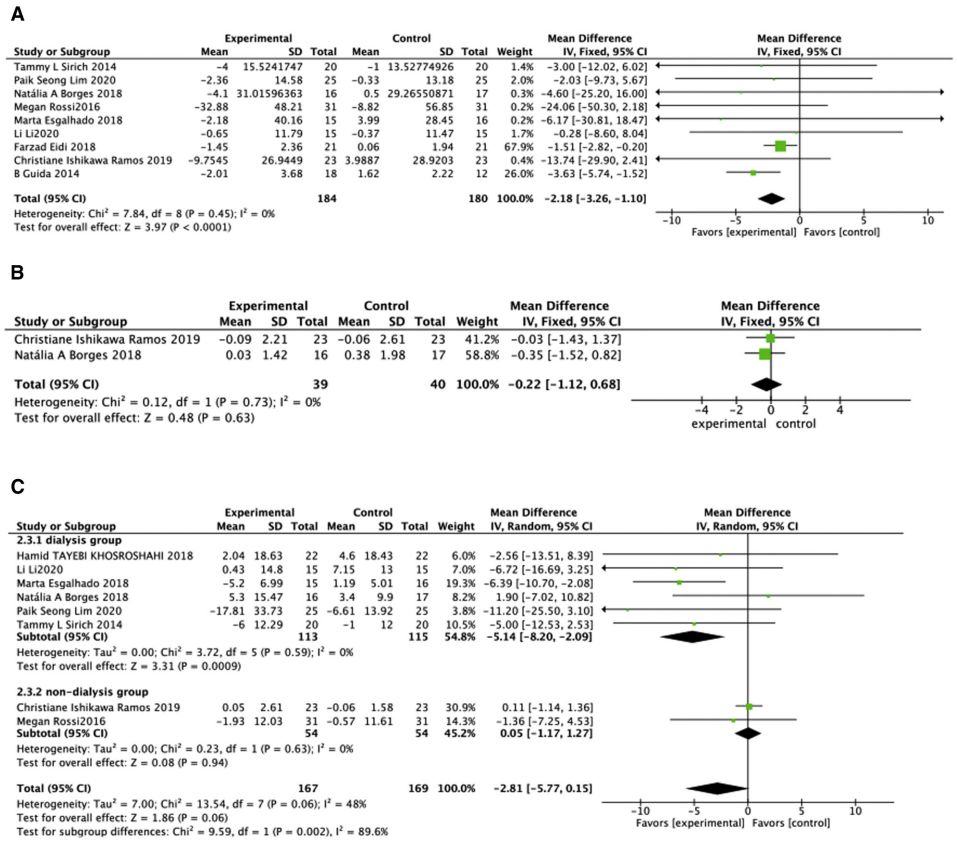
生物干预对尿毒症毒素的影响
总而言之,研究结果强调了生物制剂对 CKD 患者的肌酐、氧化应激(丙二醛、总抗氧化能力)、炎症(白细胞介素 6)和尿毒症毒素(对甲酚硫酸盐)的标志物的有利影响。生物制剂并不影响透析前或透析患者的估计肾小球滤过率、白蛋白、吲哚-3-乙酸或脂质。
参考文献:Jing Liu, JianYong Zhong, HaiChun Yang, et al. Biotic Supplements in Patients With Chronic Kidney Disease: Meta-Analysis of Randomized Controlled Trials,Journal of Renal Nutrition,Volume 32, Issue 1,2022, Pages 10-21,ISSN 1051-2276,https://doi.org/10.1053/j.jrn.2021.08.005.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照试验#
58
#荟萃#
48
#对照#
51
#renal#
48
#荟萃分析#
51
#CKD患者#
65
#随机对照试验#
51
学习了
52