Neurology:常服抗抑郁药或增加脑出血风险
2012-10-22 任海军 新华社
美国《神经病学》杂志网络版刊登一项报告说,经常服用某类广泛使用的抗抑郁药将增加服用者脑出血的风险。研究人员提醒已存在此类风险的患者可考虑使用其他类型药物。 加拿大安大略西部大学研究人员报告说,他们对包括50万名对象的16项研究汇总分析后发现,与不服药者相比,日常服用选择性血清再吸收抑制剂类抗抑郁药者颅内出血的风险高50%,出现脑溢血的风险高40%。 选择性血清再吸收抑制剂是一类抗抑
美国《神经病学》杂志网络版刊登一项报告说,经常服用某类广泛使用的抗抑郁药将增加服用者脑出血的风险。研究人员提醒已存在此类风险的患者可考虑使用其他类型药物。
加拿大安大略西部大学研究人员报告说,他们对包括50万名对象的16项研究汇总分析后发现,与不服药者相比,日常服用选择性血清再吸收抑制剂类抗抑郁药者颅内出血的风险高50%,出现脑溢血的风险高40%。
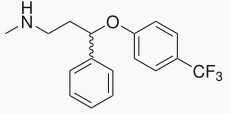
选择性血清再吸收抑制剂是一类抗抑郁药物的总称,包括百忧解等,用于治疗抑郁症、焦虑症、强迫症及神经性厌食症。这类药物在很多国家都是最常用的抗抑郁处方药,但其有效性和安全性已受到质疑。
研究负责人、安大略西部大学助理教授丹尼尔·哈克姆强调,应审慎看待分析结果,因为颅内出血和脑溢血毕竟很少见,确需服用选择性血清再吸收抑制剂的患者不应停止用药,但对已经存在这两类出血风险的人群,如抗凝血药使用者、有类似出血史者和酗酒者等,医生可以考虑使用其他类型的抗抑郁药。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








总结十分全面,到位,学习了,辛苦!
99
#Neurol#
43
#抑郁药#
32
#抗抑郁#
41