病例分享丨左侧锁骨下动脉盗血介入治疗一例
2018-06-09 柴潇 中国军网综合
锁骨下动脉盗血综合征是指在锁骨下动脉或头臂干的椎动脉起始处的近心段有部分的或完全的闭塞性损害,由于虹吸作用,引起患侧椎动脉中的血流逆行,进入患侧锁骨下动脉的远心端,导致椎-基动脉缺血性发作和患侧上肢缺血性的症候。可以有脑缺血或上肢缺血症状。

何谓锁骨下动脉盗血?
锁骨下动脉盗血综合征是指在锁骨下动脉或头臂干的椎动脉起始处的近心段有部分的或完全的闭塞性损害,由于虹吸作用,引起患侧椎动脉中的血流逆行,进入患侧锁骨下动脉的远心端,导致椎-基动脉缺血性发作和患侧上肢缺血性的症候。可以有脑缺血或上肢缺血症状。
临床表现
1.症状
一般男性较女性多见,年龄多在50岁以上,最常见的症状,如眩晕、肢体轻瘫、感觉异常、双侧视力障碍、共济失调、复视、晕厥。少见的尚有间歇性跛行、发音困难、吞咽困难、耳鸣、抽搐、头痛及精神障碍。少数可出现“倾倒症”,突然下肢肌力丧失而跌倒的发作,可以没有意识障碍,并能迅速恢复。部分患者可有上肢易疲劳、酸痛、发凉和感觉异常等,极少数引起手指发绀或坏死。
2.体征
患侧桡动脉搏动大多减弱或消失,有的肱动脉或锁骨下动脉搏动也减弱或消失。患侧上肢血压降低,双侧上肢收缩压相差一般在20mmHg以上。锁骨上窝可闻及收缩期杂音。
检查
1.经颅多普勒超声(TCD)
检测颈部血管及血流,可见椎动脉反向血流信号,疑诊者应行患侧束臂试验。
2.彩色多普勒超声
可见锁骨下动脉起始部狭窄或闭塞,狭窄处可见血流紊乱,流速增高,狭窄远端动脉则成低阻改变;椎动脉血流反向,束臂试验可增加阳性检出率。
3.CT血管成像(CTA)或磁共振血管成像(MRA)
为目前首选方法,可见椎动脉起始处近心端锁骨下动脉管壁粥样硬化斑块,管腔狭窄或闭塞,并可全面了解主动脉弓及其主要分支动脉的形态。
4.数字减影血管造影(DSA)
为诊断的金标准,可见椎动脉起始处近心端锁骨下动脉狭窄或闭塞,患侧椎动脉显影对比度下降,甚至可见造影剂经对侧椎动脉逆流至患侧椎动脉,并达锁骨下动脉的远心端。
典型的临床症状,伴患者上肢脉搏减弱,收缩压较对侧下降20mmHg以上,听诊闻及锁骨上窝杂音,诊断多不困难。结合TCD、彩超及CTA或DSA检查可明确诊断。
治疗
目前常用的外科治疗方法主要有两大类:经皮腔内血管成形术和各种解剖外旁路术。
1.经皮腔内血管成形支架置入术(PTA)
经皮穿刺输送球囊导管至锁骨下动脉狭窄或闭塞处,扩张球囊重建动脉管腔,并可行支架植入防止弹性回缩及动脉夹层等。目前已成为锁骨下动脉盗血综合征的首选治疗方法。
2.解剖外旁路重建术
包括颈动脉-锁骨下动脉、锁骨下动脉-锁骨下动脉、腋动脉-腋动脉旁路转流术等。
3.对病因为动脉粥样硬化的老年患者
可服用抗凝或抗血小板聚集剂以减少血栓形成和发展。对罕见的由巨细胞动脉炎所致者可采用类固醇治疗。
病例分享
中老年女性,因反复活动后头晕,左上肢麻凉5年,加重1周入院。既往外院彩超提示:左侧锁骨下动脉起始部狭窄,左侧椎动脉完全反向血流。查体:左上肢血压90/60mmHg ,右上肢血压140/80mmHg。左侧桡动脉搏动未扪及,余神经系统未见阳性体征。
诊断:左侧锁骨下动脉盗血综合症。
MRA示左侧椎动脉颅内段闭塞。

结合病史及检查,明确诊断后建议患者完善DSA检查,明确血管狭窄及侧枝代偿情况,必要时行支架植入术。

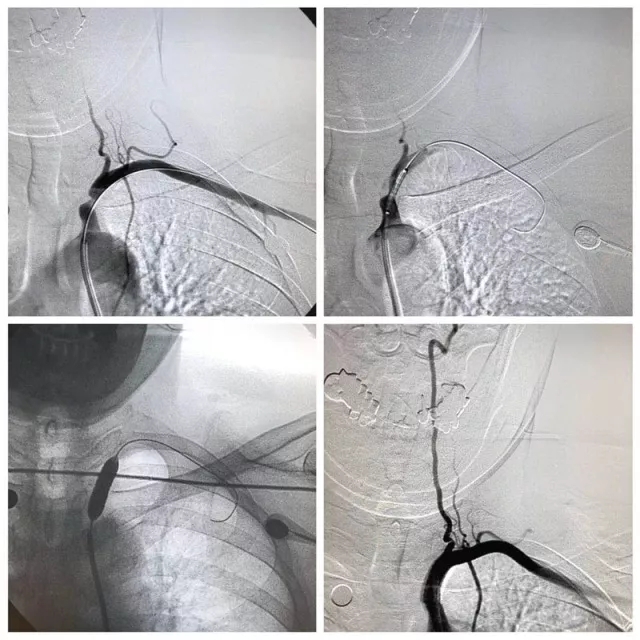
DSA:左侧椎动脉完全反向血流,左侧锁骨下起始部极重度狭窄!
DSA明确诊断后行左侧锁骨下动脉支架成形术!
顺利于狭窄段植入雅培Omnilink 8/19支架一枚,狭窄解除,血流通畅!
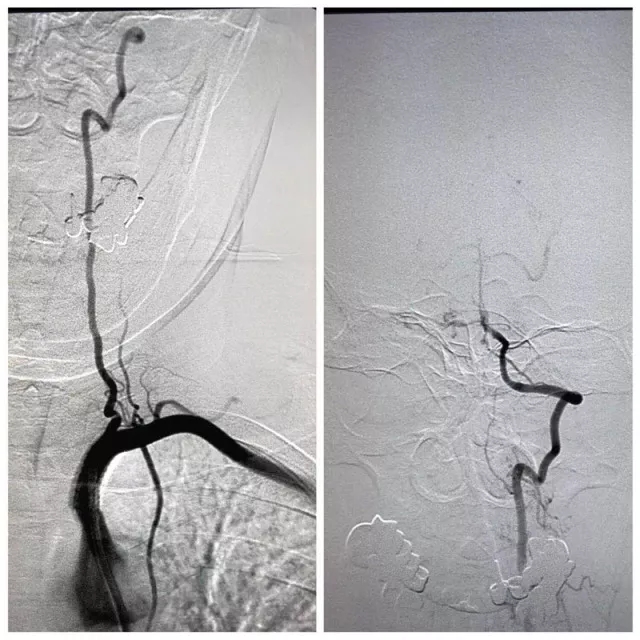
术后即刻造影:左侧椎动脉恢复正向血流,颅内血供明显改善。查体:双上肢血压120/80mmHg,左侧桡动脉搏动良好。术后患者头晕明显改善,治疗取得完美结局!
锁骨下动脉盗血是导致后循环缺血的常见病因,体检中发现双上肢血压不对称,肢体动脉搏动减弱,肢体发凉等,应该及时就诊!介入治疗锁骨下动脉盗血综合症因其微创,技术简单,风险小,恢复快,已成为首选治疗方法!
(来源:解放军第210医院 神经内科)
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#锁骨下#
47
#锁骨#
32
学习了谢谢分享!!
70
好文献学习了
74
学了
72