致心律失常性右室心肌病合并右心血栓动态演变超声表现1例
2018-11-23 刘瑜 刘勇 中国超声医学杂志
患者女,54岁。主因“间断喘憋2年余,加重3d”入院。查体:患者平卧位,脉搏70次/min,呼吸18次/min,血压103/62mmHg,口唇无发甜,双侧颈静脉怒张,双肺听诊呼吸音清,未闻及干湿啰音,心脏叩诊心界扩大,心律齐,心音低钝,三尖瓣区收缩期I级收缩期杂音。
患者女,54岁。主因“间断喘憋2年余,加重3d”入院。查体:患者平卧位,脉搏70次/min,呼吸18次/min,血压103/62mmHg,口唇无发甜,双侧颈静脉怒张,双肺听诊呼吸音清,未闻及干湿啰音,心脏叩诊心界扩大,心律齐,心音低钝,三尖瓣区收缩期I级收缩期杂音。
急诊心超示:右心明显增大,右室壁明显变薄,运动幅度弥漫性减低,右室流出道瘤样扩张(内径52mm),右心腔血流缓慢,可见浓密红细胞自发显影(图1),未见明显血栓,三尖瓣区可见大量反流信号,峰值压差25mmHg,下腔静脉扩张塌陷率消失。卵圆孔水平右向左分流。考虑:右室心肌受累性病变,致心律失常性右室心肌病。给予对症治疗,症状无缓解。

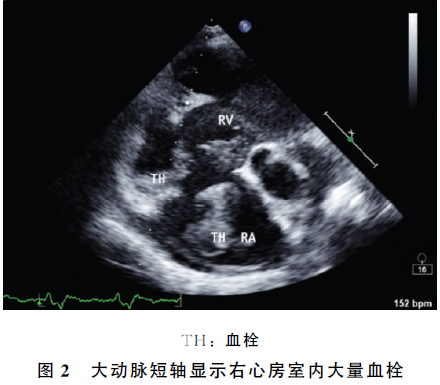
2d后复查心超示:右室、右房大量低回声非活动性附壁血栓,三尖瓣开放受限,余右心情况基本同前(图2)。予以抗凝及对症等治疗。4d后,患者病情急剧加重,突发喘憋、呼吸困难,SPO2降至50%,心超示:右室、右房血栓范围较前范围缩小,形态不规则,表面有活动性。结合临床考虑右心血栓脱落导致肺动脉栓塞。3d后患者因多器官衰竭病死。
讨论
致心律失常性右室心肌病(ARVC)是以右室心肌不同程度地被脂肪组织或纤维组织替代为特征的心肌病。ARVC患者典型超声心动图表现:不同程度的右室扩大、右室流出道增宽、室壁运动障碍以及局限性室壁瘤等,但并无明显肺动脉高压征象。
文献报告超声检查或尸检中可发现部分患者伴有附壁血栓形成,但体积多相对较小,伴有巨大血栓且快速进展者少见。本例患者在检出右室心肌受累病变基础上,短期随访超声发现右心大量附壁血栓,进而血栓脱落引发急性肺栓塞,导致病情进一步恶化,文献罕见报告。
原始出处:
刘瑜,刘勇.致心律失常性右室心肌病合并右心血栓动态演变超声表现1例[J].中国超声医学杂志,2018(03):268.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#致心律失常性#
43
#演变#
36
#超声表现#
47
#致心律失常性右室心肌病#
49
#肌病#
45
学习了
66