J Gastroenterology:磁共振成像可以评估克罗恩病患者肠粘膜是否愈合并降低手术风险
2018-10-02 MedSci MedSci原创
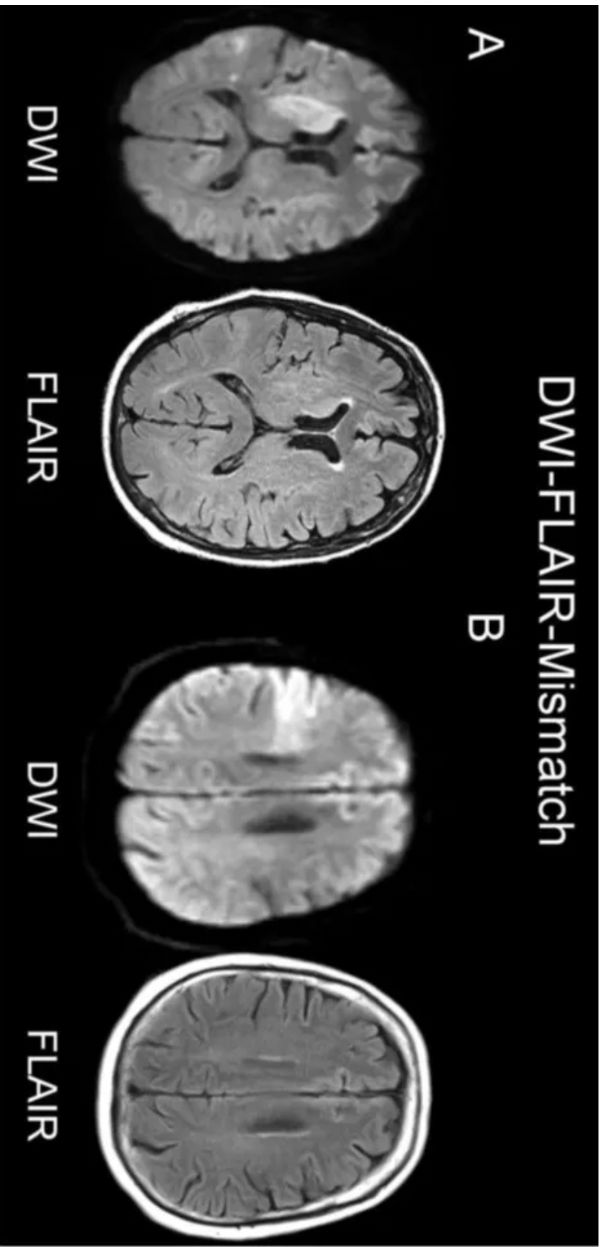
内镜下粘膜愈合被认为是克罗恩病(CD)的最佳治疗终点,因为它与更长的临床缓解结果相关。因此,有关研究人员探究了是否可以使用磁共振成像(MRI)来评估肠粘膜的愈合(BWH),并以此预测克罗恩病长期的预后结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
28
#粘膜#
33
#GAS#
32
#AST#
33
学习了
51
#磁共振#
33
#Gastroenterology#
33
#手术风险#
46