Genet Med:lumasiran治疗原发性1型高草酸尿症的3期试验:一种新的婴幼儿RNAi疗法
2022-01-30 从医路漫漫 MedSci原创
原发性高草酸尿症1型(PH1)是一种罕见的进行性常染色体隐性遗传病,其特征是由AGXT编码的肝过氧化物酶丙氨酸-乙醛酸转氨酶缺乏引起的肝草酸盐生成增加。
背景:原发性高草酸尿症1型(PH1)是一种罕见的进行性常染色体隐性遗传病,其特征是由AGXT编码的肝过氧化物酶丙氨酸-乙醛酸转氨酶缺乏引起的肝草酸盐生成增加。在丙氨酸-乙醛酸转氨酶活性降低的个体中,乙醛酸不能有效转化为甘氨酸,而是在肝脏中氧化为草酸盐,导致过多的草酸盐输送到肾脏进行排泄。过量的草酸盐与钙结合形成晶体,导致肾钙质沉着和肾结石,导致进行性肾病,最终导致许多患者肾衰竭。随着肾功能下降,草酸盐的清除减少,导致血浆草酸盐浓度升高,草酸钙沉积在组织中,包括骨、脉管系统、心脏、皮肤、眼睛和神经,导致严重的终末器官损伤,这种情况称为全身性草酸中毒。尽管PH1在任何年龄都可能出现,但肾衰竭、全身性草酸中毒和死亡率增加通常会影响儿童,2-5岁的婴儿最严重。
目的:原发性1型高草酸尿症(PH1)是一种罕见的进行性遗传疾病,治疗选择有限。我们报道了一种核糖核酸干扰治疗剂lumasiran对患有PH1的婴幼儿的疗效和安全性。
方法:这项单臂、开放标签、3期研究评估了年龄< 6岁的PH1患者的lumasiran,如果年龄≥12个月,估计肾小球滤过率> 45ml/min/1.73m3,或者如果年龄< 12个月,估计血清肌酐正常。主要终点是从基线到第6个月点尿草酸盐与肌酐比值的百分比变化。次要终点包括尿草酸盐≤1.5×正常值上限的患者比例和血浆草酸盐的变化。
结果:所有患者(18例)均完成了6个月的初步分析。中位年龄为50.1个月。斑点UOx:Cr的最小二乘平均减少百分比为72.0%。第6个月,50%的患者(9/18)达到斑点UOx:Cr ≤1.5×正常值上限。血浆草酸盐的最小二乘平均减少百分比为31.7%。最常见的治疗相关不良事件是短暂、轻微的注射部位反应。
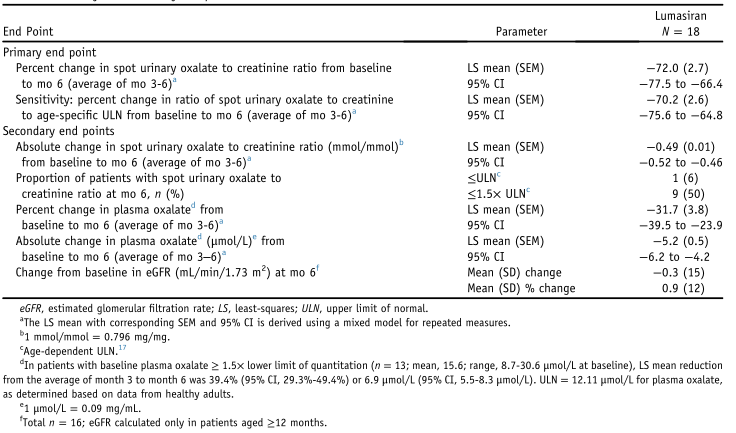
表1 主要和次要终点

图1 来自BL的Lumasiran每次就诊时尿草酸/肌酐比值的百分比变化,平均值(±SEM)。
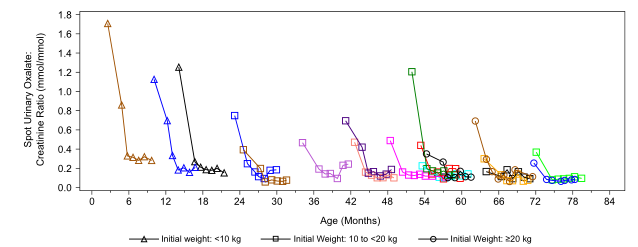
图2 尿草酸与肌酐之比照年龄之实际值。1 mmol/mmol = 0.796 mg/mg。

表2 安全性
结论:Lumasiran显示,在<6岁的PH1患者中,斑点UOx:Cr和血浆草酸盐快速、持续下降,安全性良好,这表明RNA干扰疗法是婴幼儿安全、有效的治疗方案
原文出处:Sas DJ, Magen D, Hayes W,et al.Phase 3 trial of lumasiran for primary hyperoxaluria type 1: A new RNAi therapeutic in infants and young children.Genet Med 2021 Dec 07
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Gene#
0
#RNAi#
45
#原发性1型高草酸尿症##RNAi疗法#
0
#原发性#
50
#Genet#
47
#NET#
47
#3期试验#
53
#Med#
35