European Radiology:AI在BI-RADS 0类乳腺钼靶病变方面的附加价值
2021-11-09 shaosai MedSci原创
乳腺癌是全世界范围内最常见的女性恶性肿瘤,而乳腺钼靶检查是检测早期乳腺癌的主要方式和有效途径。

乳腺癌是全世界范围内最常见的女性恶性肿瘤,而乳腺钼靶检查是检测早期乳腺癌的主要方式和有效途径。为了评估癌症风险,美国放射学会建立了乳腺成像报告和数据系统(BI-RADS)来对乳腺病变进行分层。BI-RADS报告系统使放射科医生能够清晰、一致地将结果传达给转诊医生,并给出最终评估和具体建议。
BI-RADS 1代表阴性发现,2代表良性发现,3-6意味着恶性的概率越来越大。特别是,当乳腺钼靶检查无法评估,需要进一步的影像学检查进行诊断时,该病变则被定义为BI-RADS 0。进一步的影像学检查是提高BI-RADS对乳腺病变分类诊断性能的有效方式[。然而,这些程序则会增加患者的焦虑和检查费用。
近年来,使用基于深度学习技术(主要是深度神经网络)的人工智能(AI)系统在各种医学图像分析任务中获得了巨大成功。具体来说,大量的研究已经证明了乳腺钼靶的病变检测性能非常出色。此外,基于深度学习的人工智能系统在识别乳腺钼靶中的乳腺癌方面也能取得优于放射科医生的表现。然而,据我们所知,目前还没有关于人工智能系统协助放射科医生评估或判析BI-RADS 0病例能力的相关研究。
近日,发表在European Radiology杂志的一项研究探讨了人工智能乳腺钼靶诊断系统在协助放射科医生提高BI-RADS 0病例的评估准确性方面的价值,为提高放射科医生的诊断一致性以及患者的诊断准确性提供了技术支持及保障。
本研究纳入了2011年1月至2019年1月期间收集的34654份连续的数字乳腺钼靶研究,其中,来自1010名初始评估为BI-RADS 0患者中的1088例在2年的随访期间被召回,并用于本研究中。两位中级放射科医生在本研究开发的AI系统的协助下,对这些BI-RADS 0病例进行了回顾性的重新评估。此外,四名初级放射科医生被分成两组,分别对80个有人工智能和没有人工智能的病例进行交叉阅读。以随访诊断或活检结果为参考标准,对诊断效果进行了评估。
在1088个病例中,有626个实际上是正常的(BI-RADS 1,不需要召回)。在人工智能系统的协助下,351(56%)和362(58%)个正常病例被两位中级放射科医生正确识别,因此可以避免不必要的随访。然而,他们分别错过12个(10个浸润性癌症和2个导管原位癌)和6个(浸润性癌症)的恶性病变。这些遗漏的病变并不是高度恶性的肿瘤。引入AI后,入门级放射科医生的评分间可靠性从0.20提高到0.30(P < 0.005)。
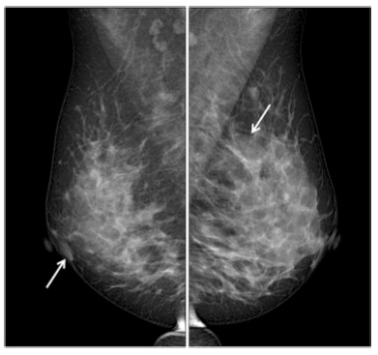
图 一名47岁的女性患者。左图:R-MLO视图。放射学报告显示,右乳在乳晕区有一个肿块(箭头所指)(BI-RADS 2)。右图。L-MLO视图。左侧乳房有不对称的高密度(箭头,BI-RADS 0)。AI系统没有在两个乳腺中发现任何异常。随访的超声检查证明两个乳腺均为阴性(BI-RADS 1)。
本研究表明,人工智能系统可为BI-RADS 0乳腺钼靶的诊断性能的提高方面的提供较高的附加价值。本研究发现,人工智能系统可以协助中级放射科医生有效地减少不必要的随访,且不会造成高度恶性肿瘤的漏诊。综上所述,本项研究可以促使人们进一步发展和了解人工智能系统在提高不确定的BI-RADS 0乳腺钼靶病变的临床决策方面的作用。
原文出处:
Chunyan Yi,Yuxing Tang,Rushan Ouyang,et al.The added value of an artificial intelligence system in assisting radiologists on indeterminate BI-RADS 0 mammograms.DOI:10.1007/s00330-021-08275-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#RADS#
32
#PE#
44
#ADS#
40
#BI-RADS#
44
学习了
86