CGH:择期剖腹产可降低HBV母婴垂直传播率
2013-10-11 daerwen2008 dxy
研究要点: 1.本研究对1409例HBsAg阳性母亲所生的婴儿数据进行回顾性分析,与正常产道分娩和紧急剖腹产相比,择期剖腹产HBV母婴垂直传播发生率显著降低。 2.HBeAg阳性且分娩前HBV DNA水平≥1,000,000 拷贝/毫升的母亲择期剖腹产,可降低母婴垂直传播率。 通过适当的被动和主动免疫可能阻断HBV的母婴传播,但HBeAg阳性高病毒血症的产妇所生婴儿的HBV母婴传播率仍达5%
研究要点:
1.本研究对1409例HBsAg阳性母亲所生的婴儿数据进行回顾性分析,与正常产道分娩和紧急剖腹产相比,择期剖腹产HBV母婴垂直传播发生率显著降低。
2.HBeAg阳性且分娩前HBV DNA水平≥1,000,000 拷贝/毫升的母亲择期剖腹产,可降低母婴垂直传播率。
通过适当的被动和主动免疫可能阻断HBV的母婴传播,但HBeAg阳性高病毒血症的产妇所生婴儿的HBV母婴传播率仍达5%-10%。目前对于选择何种分娩方式可有效降低HBV母婴传播发生率尚存争论。来自美国Mount Sinai医学院的CALVIN Q. PAN教授和中国首都医科大学佑安医院的段钟平教授等对此进行了研究。研究结果认为:HBeAg阳性且分娩前HBV DNA水平≥1,000,000 拷贝/毫升的产妇择期剖腹产可降低HBV母婴垂直传播率。该结果发表在2013年10月的《临床肠胃病学与肝脏病学》(Clinical Gastroenterology and Hepatology)杂志上。【原文下载】
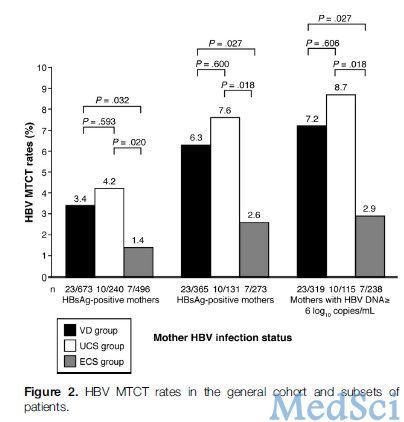
该研究主要评估了择期剖腹产分娩对HBsAg阳性的产妇HBV母婴传播率的影响。研究对1409例HBsAg阳性母亲所生的婴儿数据进行回顾性分析,673例通过正常分娩(VD),496例择期剖腹产(ECS),240例通过紧急剖腹产(UCS)。所有的婴儿接受乙型肝炎疫苗免疫,在7到12个月龄时检测到HBsAg阳性的婴儿视为母婴传播阻断失败。
研究结果显示,HBV感染母婴传播率分别为:择期剖腹产<正常产道分娩<紧急剖腹产。与正常产道分娩相比,紧急剖腹产对垂直传播没有影响。对于HBV DNA水平<1,000,000拷贝/ 毫升的产妇来说,不管采取何种分娩方法均不发生HBV母婴传播。各组间母亲或婴儿的发病率和死亡率无显著差异。
该研究结果表明:与正常产道分娩和紧急剖腹产相比,择期剖腹产HBV感染母婴垂直传播发生率显著较低。HBeAg阳性且分娩前HBV DNA的水平≥1,000,000 拷贝/毫升的母亲择期剖腹产,可降低母婴垂直传播率。
研究背景:
全球慢乙肝感染约4亿人,15%-30%的慢乙肝患者可发展为肝硬化和肝癌。在中国,有1亿多的HBV携带者,其中大多数育龄期妇女处于慢乙肝免疫耐受期,母婴传播是HBV感染的最常见途径之一。据估计,高病毒血症的母亲所生的婴儿约有10%-20%标准免疫预防失败,从而造成新生儿的感染。在以往的研究中,不同分娩方式的HBV母婴传播率得出不同的结果。为了更好地了解择期剖腹产对母婴传播率的潜在影响,特进行此研究。
本研究为回顾性分析,对于HBsAg阳性母亲,比较经正常产道分娩(VD),择期剖腹产(ECS)或紧急剖腹产(UCS)HBV母婴传播率的差异,并对HBeAg阳性和高病毒血症母亲的亚组进行分层分析。评估的主要结果是婴幼儿的乙肝表面抗原状态。HBsAg阳性年龄为7-12个月的婴儿被认为有慢性乙肝感染。母婴传播率定义为:队列研究中婴儿感染慢乙肝的比例。此外,对不同分娩方式母亲和婴儿的并发症,发病率和死亡率在进行评估。
研究结果显示,整个研究队列的HBV母婴传播率为2.8%。进一步的亚组分析:①在764例HBeAg阳性母亲中,总的HBV母婴传播率为5.2%,择期剖腹产组母婴传播率为2.6%,低于正常产道分娩组和紧急剖腹产组。②在高病毒血症母亲中,总的HBV母婴传播率为6.0%,择期剖腹产组母婴传播率为2.9%,低于正常产道分娩组和紧急剖腹产组。在研究期间没有发生母亲或婴儿死亡。
总之,择期剖腹产可降低HBV母婴垂直传播率,且在1年随访期间内并未提高母亲和婴儿的死亡率和并发症发生率。因此,无论产妇HBeAg状态如何,对产前HBV DNA水平≥106拷贝/毫升的高病毒血症的母亲进行择期剖腹产是可行的。可能需要进一步前瞻性随机对照试验证实此结论。
原文检索
Pan CQ, Zou HB, Chen Y, Zhang X, Zhang H, Li J, Duan Z.Cesarean section reduces perinatal transmission of hepatitis B virus infection from hepatitis B surface antigen-positive women to their infants.Clin Gastroenterol Hepatol. 2013 Oct;11(10):1349-55【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HBV#
45
#CGH#
36
#母婴#
36
#垂直传播#
44