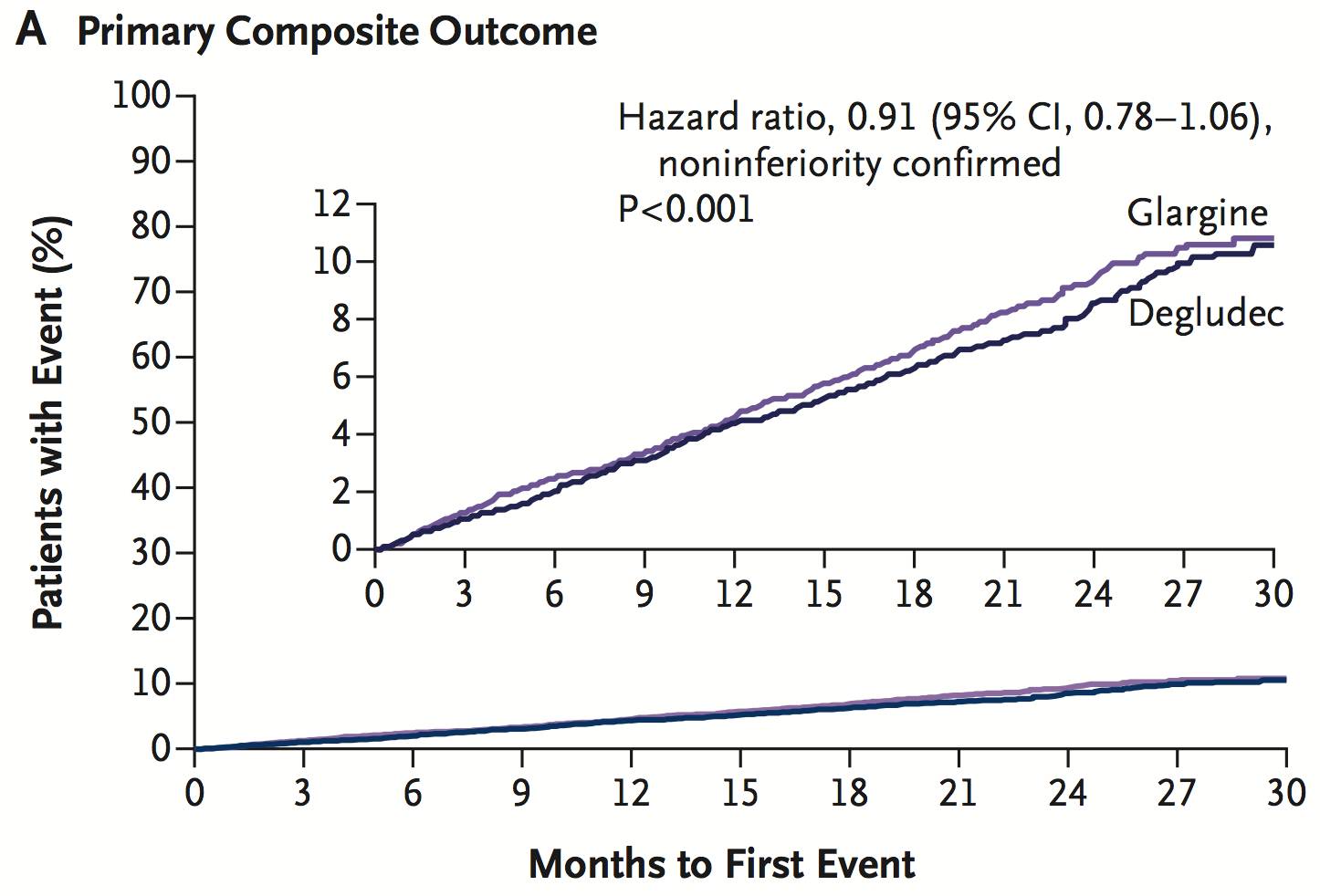
JCEM:作用于胰岛素受体的人单克隆抗体——X358,安全性和耐受性良好
2017-06-17 MedSci MedSci原创
在糖尿病治疗方面,胰岛素分泌功能受损的患者需要一种新颖的改良的治疗模式。传统的单克隆抗体在配体 - 受体结合位点结合,以提供完全活化或类似开关的抑制。然而,受体也有很多位点,称为变构位点,它就像调节开关一样调节配体 - 受体之间相互作用。目前的研究已经发现了胰岛受体三种不同类别的变构抗体,并且他们发挥不同的作用。X358是一个作用于胰岛素受体(INSR)的人源性单克隆抗体,是胰岛素信号转导时的负别
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#克隆#
36
#胰岛#
43
#JCE#
41
#JCEM#
34
#耐受性#
43
学习并分享!!!
75
学习了,受益匪浅。
59
单X358输注治疗的耐受性良好,并在胰岛素敏感性方面导致剂量依赖性降低。X358治疗高胰岛素血症和低血糖状态的临床开发仍在进行中。
65
学习了,感谢分享。
60