步骤详解!复合面部提升技术带来很好的亚洲人面部提拉效果
2022-01-01 MedSci原创 MedSci原创
面部组织提升技术主要分为两类:仅在SMAS层进行的解剖和提升技术;以及SMAS层以下解剖的深平面提升技术:复合皮瓣提升技术。
面部组织提升技术主要分为两类:仅在SMAS层进行的解剖和提升技术;以及SMAS层以下解剖的深平面提升技术:复合皮瓣提升技术。
随着对面部解剖学的理解不断进步,使得浅表肌肉腱膜系统(SMAS)解剖越来越安全,复合式面部整容术也越来越流行。
本文介绍了新加坡团队在亚洲患者中进行复合面部整容的技术,并回顾了他们的经验和结果。
图1 文章来源
研究者在2010年1月至2020年6月,对128名亚洲患者进行了复合式面部提升术。94例为一期整容,34例为二期或三期整容。
作者的手术技术和适应亚洲患者的具体要求进行了详细描述。
面部软组织分为五层:
- 1.皮肤
- 2.皮下组织
- 3.SMAS层:主要分布于面颊外侧、眶周的眼轮匝肌及面颈前内侧的颈阔肌
- 4.韧带及疏松间隙:司 固定及滑动
- 5.深筋膜层:咀嚼肌、颞肌及咬肌表面的深筋膜及深层骨膜

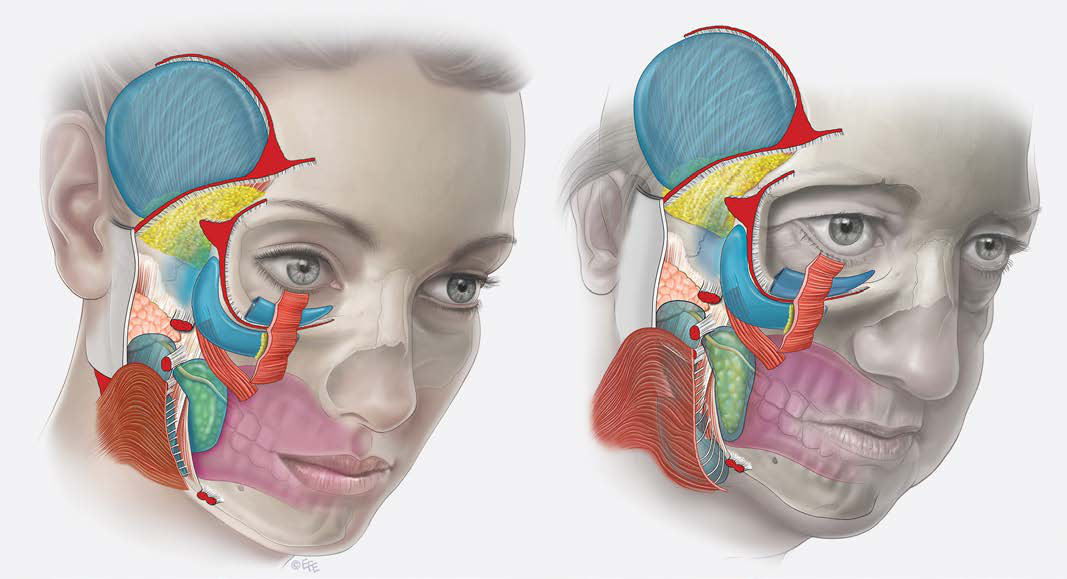
图2、3 皮肤分层图解,年龄对比
第4层是复合浅筋膜和深筋膜与下方咀嚼器之间的自然滑动面。在年轻人中,这一层虽然允许移动,但很坚固且拉紧(左)。随着年龄的增长,由于松弛和组织松弛的倾向,面部软组织空间的顶部会出现扩张和下垂(右)。因此,由于这是随着年龄增长而形成的松弛的主要解剖部位,直接收紧浅筋膜是进行面部整容的最有效和最合理的方法。这也通过将浅筋膜恢复到年轻时的位置,实现了最自然、最和谐的面部年轻化
因此,切开第4层,拉动整个浅筋膜的复合皮瓣以实现面部提升技术叫做复合面部提升技术。
手术步骤主要为切口及标记、打开SMAS下的间隙及松解韧带(下咬肌前间隙)、去除多余的颊脂垫、打开颧前间隙、打开颈阔肌间隙,而后用3-0线提升下咬肌前间隙的顶层、上咬肌前间隙的顶层、颧弓韧带、颧弓间隙的顶层。
其中做切口时要注意:
切口注意隐蔽及无痕;画好过渡标记:从外眦至下颌角,二者平滑的连线即为过渡线;耳周切口处开始分离,起始层次为皮下组织层,沿SMAS层表面向前分离。
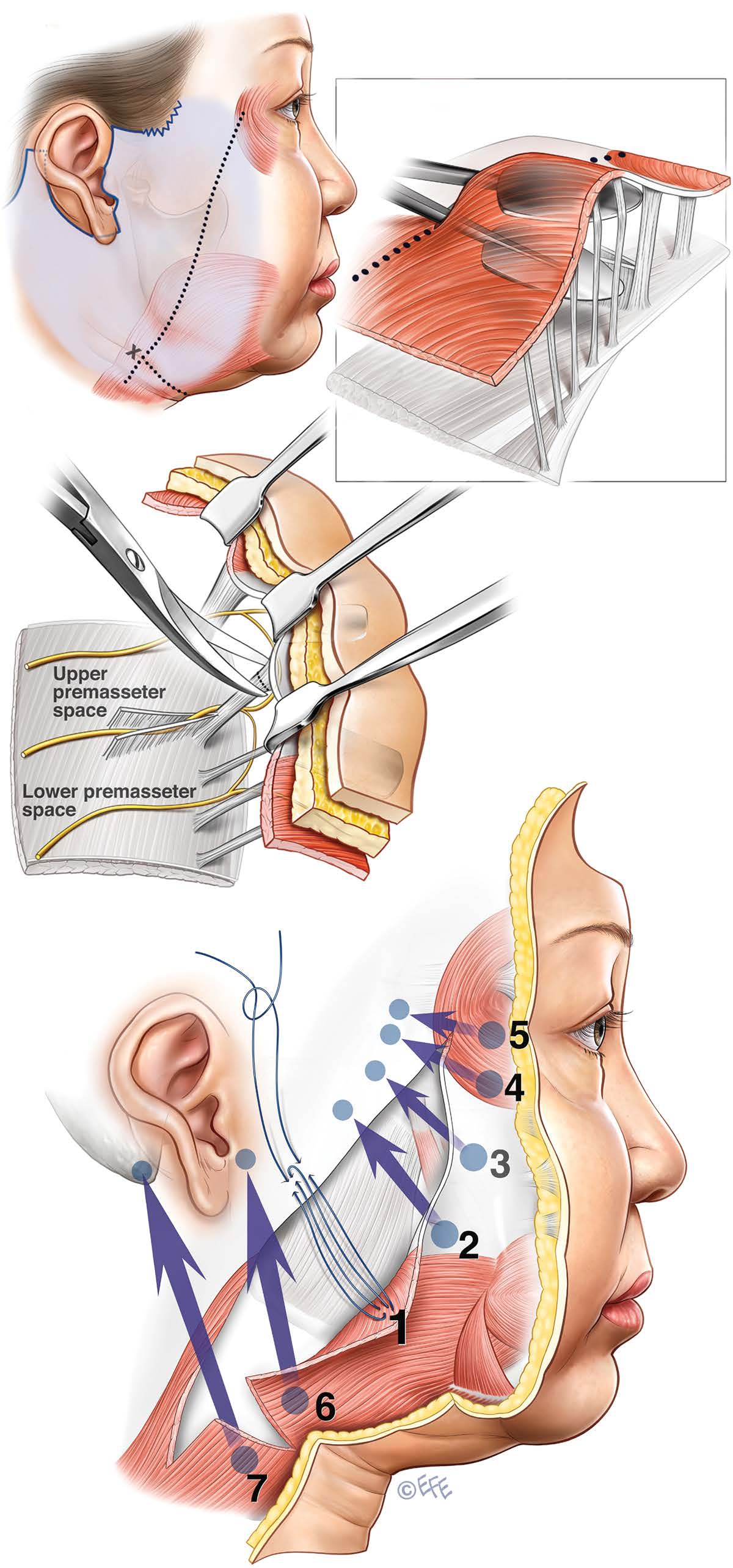
图4 步骤图解
此图显示了面部的第4层(亚SMAS)解剖结构。术者以三步方法松解SMAS。第第1步是在下表面进行解剖,通过释放分离下表面和上表面的固定韧带进入下表面和上表面的装配前间隙。较低的预装配空间最宽,最容易进入。然后打开上部空间,两个空间都缩回,它们之间的固定韧带可以急剧释放。在这里,面神经的下颊支在腮腺肉瘤筋膜下运行,因此保留韧带的释放应在软组织间隙顶部的高度进行。第2步通过眼轮匝肌下钝性剥离并打开颧前间隙,将剥离引导至松解的上部。钝性手指解剖可用于完全打开鼻唇皱襞的空间(FAME、手指辅助颧骨提升术、技术)。第3步是迅速释放颧骨保留韧带的关键步骤。因为这里没有面部软组织间隙,所以必须通过锐利的解剖来完成释放。为安全起见,将牵开器分别放置在该区域上方和下方颧前间隙和装配前间隙顶部下方的间隙中,以使颧骨韧带处于张力状态。由于神经位于解剖的底部,因此在离间隙顶部更近的高处进行释放,释放颧骨韧带,并在颧骨大肌上向鼻唇沟方向进行解剖,将神经安全地放在解剖的地板上。这种程度的释放允许面部复合皮瓣完全活动。
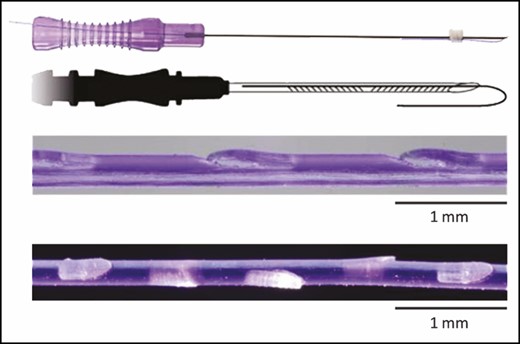
平均随访26个月(6-108个月)。脂肪移植是手术的一个组成部分,95%的患者同时接受面部脂肪移植和面部整容。
结果显示,大多数患者对该技术的美学效果表示高度满意,效果自然、持久。剥离的面部提升平面穿过面部软组织间隙,提供非创伤性SMAS下通路,精确释放中间的保留韧带,以有效移动皮瓣。通过强调复合皮瓣的张力而不是皮肤闭合处的张力,绝大多数患者的疤痕是离散的。并发症少,无血肿或皮瓣坏死。暂时性神经损伤率为1.5%,没有患者有永久性神经损伤。
综上述,复合式面部提升术是亚洲患者的理想技术,因为它能提供自然、持久的效果;迅速恢复;患者满意度高。
原始文章:
Wong Chin-Ho,Hsieh Michael Ku Hung,Mendelson Bryan,Asian Face Lift with the Composite Face Lift Technique.[J] .Plast Reconstr Surg, 2021, undefined: undefined.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
42
学习
44
厉害了
50
学习
62
增长知识了
49
学习了,谢谢分享
34
向研究表明,在一次就诊时被确定为MCI的人中,有5%至53%在下一次就诊时不再
41