CGH:较高的抗肿瘤坏死因子-α水平与克罗恩肛周瘘的放射学结果改善相关
2022-05-30 xuyihan MedSci原创
克罗恩病患者更常见的是肛门周围出现皮赘,有时与痔难于区分,因此应找医生仔细检查,分清楚是痔还是皮赘。 皮赘的大小、形状、性质各异。有些比较大、伴有水肿、质硬、紫色,有些像“大象耳朵”,扁平。
肛周瘘管克罗恩病是一种使人生活质量严重受损的疾病,约30%罗恩病的患者都受此疾病的影响。在人群研究中结肠和直肠疾病受累的患者更容易患有此病。手术和药物治疗的结合是目前的标准治疗方案,但只有三分之一的患者能达到持久的缓解。但只有三分之一的患者的复杂肛周瘘得到了持久的缓解。抗肿瘤坏死因子药物,特别是英夫利昔单抗和阿达木单抗,仍然是目前治疗的主流药物。越来越多的证据表明,较高的抗TNF药物水平与临床结果的改善有关。但尚不清楚这是否会改善放射学评估的愈合。本项研究旨在评估抗TNF药物水平与肛周瘘克罗恩病放射学结果之间的关联。
为此,研究人员进行了一项横断面回顾性多中心研究。纳入的患者为接受维持英夫利昔单抗或阿达木单抗治疗的肛周瘘克罗恩病患者,收集了患者6个月内的肛周磁共振成像和药物水平。在药物水平和影像学之间接受剂量变化或瘘管手术的患者被排除在本项研究分析之外。使用 Van Assche 指数对放射疾病活动进行评分,使用以下指数计算炎症子评分:T2 加权成像高信号,瘘管> 3 mm直径,直肠壁受累。主要观察终点是放射愈合(炎症子评分≤6)。次要终点是放射学缓解(炎症子评分 = 0)。
在193名患者(英夫利昔单抗,n=117;阿达木单抗,n=76)中,放射愈合患者的中位药物水平高于活动性疾病患者(英夫利昔单抗 6.0 vs 3.9 μg/mL;阿达木单抗 9.1 vs 6.2 μg/mL;P < .05)。与活动性疾病患者相比,放射学缓解患者的中位药物水平也更高(英夫利昔单抗 7.4 vs 3.9 μg/mL;P<.05;阿达木单抗 9.8 vs 6.2 μg/mL;P=.07)。具有较高抗 TNF 药物水平三分位数的中位炎症子评分显着降低。
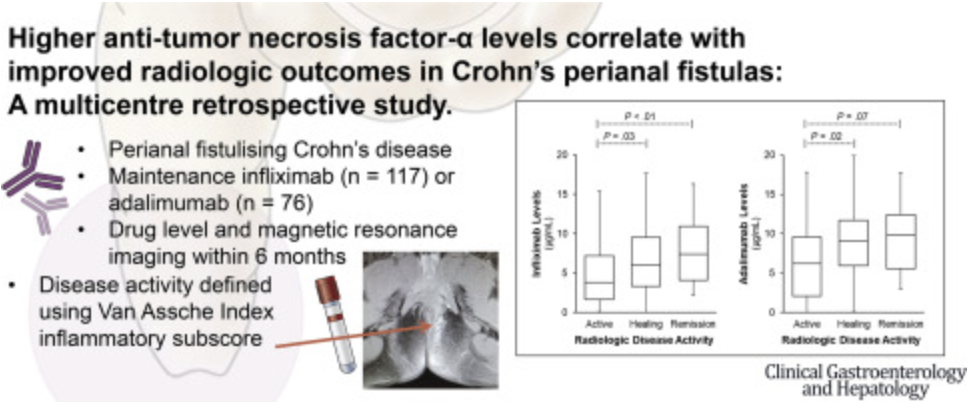
图:抗肿瘤坏死因子-α水平与克罗恩肛周瘘的放射学结果的相关性示意图
本项研究证实较高的抗 TNF 药物水平与改善肛周克罗恩病磁共振成像的放射学结果相关,英夫利昔单抗和阿达木单抗在较高药物水平三分位数上的治疗效果改善逐渐增加。
原始出处:
Michael De Gregorio. Et al. Higher Anti-tumor Necrosis Factor-α Levels Correlate With Improved Radiologic Outcomes in Crohn’s Perianal Fistulas. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CGH#
40
#肛周瘘#
43
#坏死#
49
#放射学#
38
#肿瘤坏死因子#
0
#抗肿瘤坏死因子#
29
#抗肿瘤坏死因子#
26