宝宝低血糖了!怎么办?
2016-09-11 @白衣奶爸 医学界儿科频道
新生儿低血糖症是指新生儿血糖值低于正常新生儿最低血糖值,许多疾病都会导致新生儿低血糖,低血糖可以导致脑细胞失去基本能量来源,脑代谢和生理活动无法进行,如不及时干预纠正,会造成永久性脑损害!遗留神经系统后遗症!因此,作为一名临床医生,应该对新生儿低血糖的处理,高度重视,及时诊断和治疗。新生儿低血糖症的诊断:美国新生儿低血糖管理指南:新生儿出生 24 h 内,血糖水平应持续 > 2. 5 mmo
新生儿低血糖症是指新生儿血糖值低于正常新生儿最低血糖值,许多疾病都会导致新生儿低血糖,低血糖可以导致脑细胞失去基本能量来源,脑代谢和生理活动无法进行,如不及时干预纠正,会造成永久性脑损害!遗留神经系统后遗症!因此,作为一名临床医生,应该对新生儿低血糖的处理,高度重视,及时诊断和治疗。
新生儿低血糖症的诊断:
美国新生儿低血糖管理指南:新生儿出生 24 h 内,血糖水平应持续 > 2. 5 mmol/L ; 出生 > 24 h,血糖水平应持续 > 2.8 mmol/L,低于上述水平,则为低血糖。
我国目前较为公认的标准:多主张不论胎龄和日龄,低于2.2 mmol/L,诊断低血糖症,而低于2.6 mmol/L,为临床需要处理的界限值。
新生儿低血糖症的病因:
1、暂时性低血糖症:多数病例为生后暂时性低血糖,主要原因有:
1)糖摄入减少:新生儿因喂养、生病等因素,导致糖量摄入少;
2)糖消耗过多:患病的新生儿糖量消耗大,容易发生低血糖症,如新生儿窒息、感染、酸中毒等容易并发低血糖症;
3)糖原储存不足:早产儿、低于胎龄儿糖原储存不足,加上原发疾病导致摄入少、消耗大,低出生体重儿并发低血糖症几乎达到30%-50%,甚至更多;
4)糖尿病母儿:出生后葡萄糖来源中断,而胰岛素水平较高,极易发生新生儿低血糖症。
2、持续性低血糖:
1)高胰岛素血症;
2)先天性代谢疾病:糖代谢障碍、糖原累积病、半乳糖血症;氨基酸代谢疾病、脂肪代谢疾病等;
3)内分泌疾病:垂体功能低下、皮质醇缺乏症、肾上腺素缺乏症等。
新生儿低血糖症的临床表现:
新生儿低血糖症多为无症状型。
出现症状者,多表现为:精神萎靡、嗜睡、喂养困难、肌张力低下、呼吸暂停、阵发性青紫,也可以表现为烦躁、震颤、惊厥。
新生儿低血糖症的处理原则:
积极预防,高危儿出生后30分钟尽快检测血糖,早期喂养或必要时静脉营养;如出现低血糖,尽快评估病情,分析病因,积极诊治!
可参考以下2个流程图:
1、美国2010版新生儿低血糖管理指南:
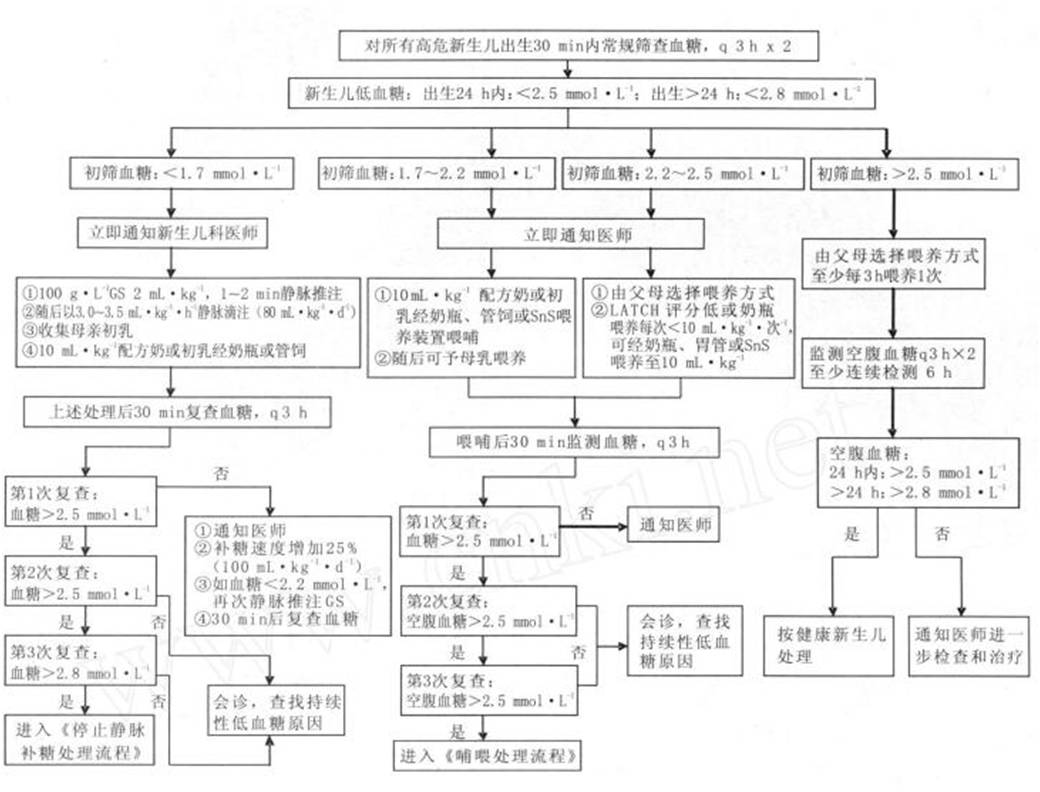
(点击图片可查看大图)
2、简化版(供参考):

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了,赞一个!!!
59
学习了,赞一个!!!
75
学习了,赞一个!!!
69
#宝宝#
30