梅斯作为媒体参加2016 AACR癌症研究新视野大会:肿瘤异质性和肿瘤代谢专题介绍以及大会日程
2016-11-01 MedSci MedSci原创
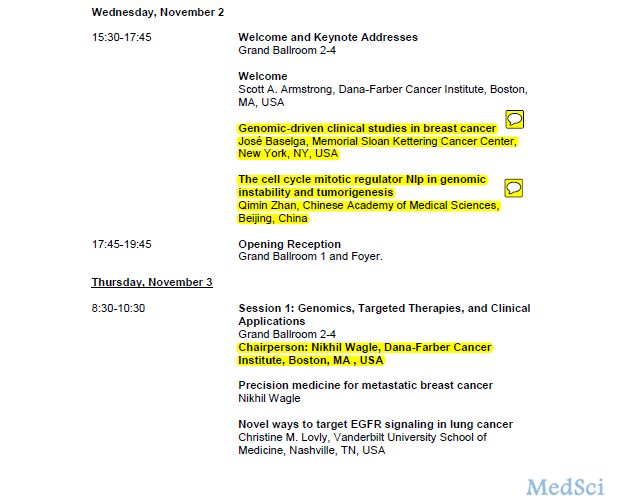
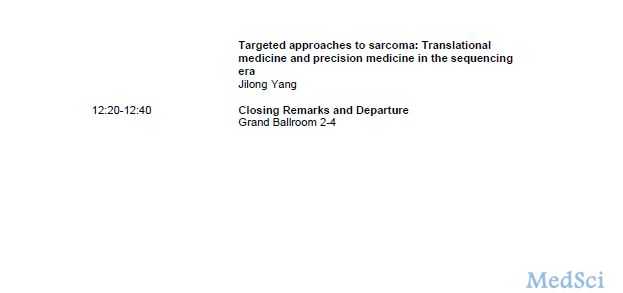
期待已久的第三届AACR癌症研究新视野大会即将于11月2日-5日在上海召开!大会吸引了来自全世界超过400名研究人员,会议期间还将展出组委会专家精选的100多幅学术海报。本次大会由7个专题会议组成,专家们将和大家探讨从实验室研究到临床治疗的整个癌症研究领域的诸多课题。同时,我们还将展示2016年AACR全球年会上发表的重要的癌症科学和医学最新研究成果。 本次大会将围绕“通过癌症科学寻

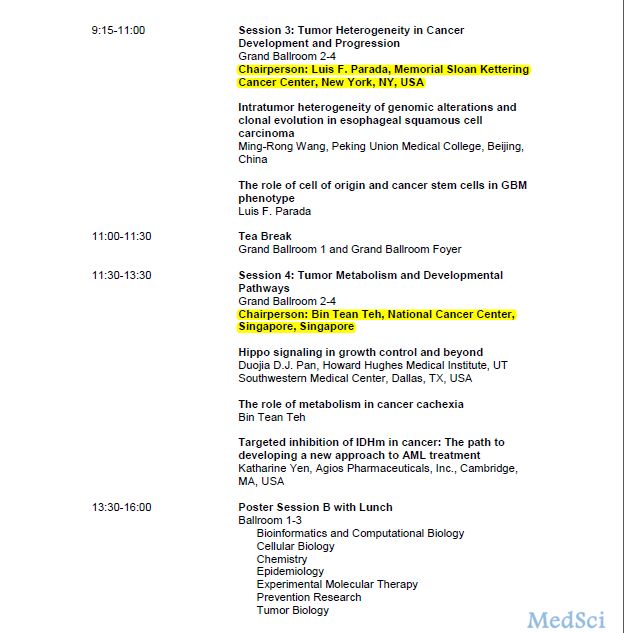
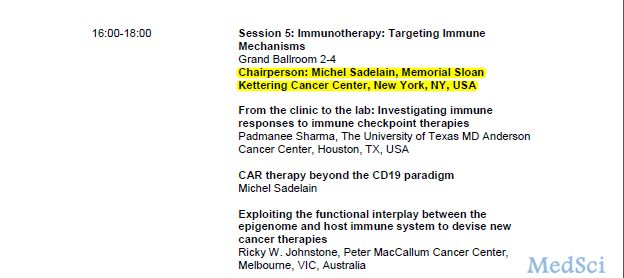
本次大会将围绕“通过癌症科学寻找治愈方案”这一主题,重点介绍癌症研究各个重要领域最新和最振奋人心的研究成果,为来自全世界各地的研究人员提供宝贵的交流机会。其中的两个专题,将介绍癌症研究的新领域:肿瘤异质性和肿瘤代谢。我们都知道癌症研究新领域的研究推动着癌症新疗法的诞生和发展。介时会议专题3:“癌症发展和进程的肿瘤异质性”的主持人Luis F. Parada博士及会议专题4:“肿瘤代谢和发展路径”的主持人Bin Tean Teh博士会为大家带来癌症研究新领域的精彩演讲。

北京协和医学院分子肿瘤学国家重点实验室教授王明荣博士将为会议专题3:“癌症发展和进程的肿瘤异质性”作主题为“食管鳞状细胞癌基因组改变的瘤内异质性和克隆演化”开场演讲。Parada博士随后会发表演讲,主题为“源细胞和癌症干细胞对GBM表型的作用”。作为一名发展生物学家,Parada博士是纽约纪念斯隆-凯特琳癌症中心脑肿瘤中心主任。他的实验室使用基因工程小鼠模型研究神经纤维瘤、脑肿瘤、癌症干细胞和肿瘤进展。

在会议专题4:“肿瘤代谢和发展路径”中我们将迎来多位德高望重的科学家与大家分享他们的研究成果,Duojia D. J. Pan博士、Bin Tean Teh博士和Katharine Yen博士。Pan博士是德克萨斯大学西南医学中心生理学系的教授和系主任,他的演讲讲题是“Hippo信号通路对生长控制和其他方面的作用”。Pan博士是Hippo信号通路路径研究方面的开拓者,Hippo信号通路是一种进化式保守发展路径,控制动物的器官尺寸。Teh博士,新加坡国立癌症中心研究室副主任,将发表题为“新陈代谢对癌症恶病质的影响”的演讲。Teh博士的研究重点是亚洲癌症基因组学,在过去的5年里,他在诸多癌症研究方面取得不俗的成果,如胆管癌、膀胱癌和乳腺肿瘤。这个环节的会议最后,Yen博士在带了来题为“癌症IDHm的靶向抑制:AML治疗新方法的开发路线”的演讲。Yen博士是Agios制药公司临床试验部门主任,她带领IDH生物和转化医学研究团队开发了目前临床试验中运用的三种IDH突变体抑制剂:AG-221、AG-120和AG-881。




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#专题#
28
感谢分享一下!
65
#梅斯#
33
#ACR#
29
#癌症研究#
34
#AACR#
30