Lancet Respir Med:ARDS—呼吸病学2015年度总结和未来10年重点研究展望专题
2015-12-01 MedSci MedSci原创
2015年继续这种乐观趋势,发表了一系列重要的随机对照试验研究结果,例如高流量鼻导管吸氧、对机械通气气压管理策略的重要性数据的二次分析、有关ARDS临床和生物异质性的新见解、可以产生新疗法的肺再生医学研究等。
近十年来ARDS临床试验都报告阴性结果,过去几年的研究又点燃了人们对于进一步降低ARDS( acute respiratory distress syndrome ,急性呼吸窘迫综合征)的新希望,例如神经肌肉阻滞和受体定位、再生医学和分子表型等等。
2015年继续这种乐观趋势,发表了一系列重要的随机对照试验研究结果,例如高流量鼻导管吸氧、对机械通气气压管理策略的重要性数据的二次分析、有关ARDS临床和生物异质性的新见解、可以产生新疗法的肺再生医学研究等。
1.高流量鼻导管吸氧
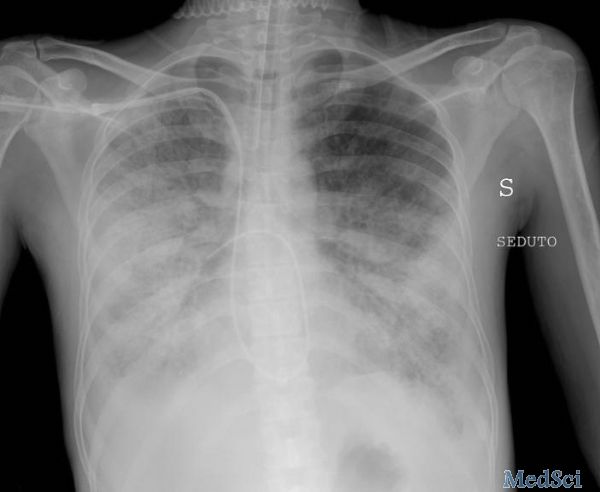
多中心FLORALI试验比较310例早期急性I型呼吸衰竭患者使用高流量鼻导管吸氧、常规面罩或无创机械通气。虽然这些患者不符合ARDS柏林定义(因为受试者不接收气道正压机械通气),受试者氧合指数<300mmHg,244例(79%)受试者胸片显示两侧肺浸润,大多数受试者符合欧美共识会议急性肺损伤的定义。
主要预后(28天内气管插管率)在三个治疗组之间没有显著性差异(高流量鼻导管吸氧 38%,常规面罩吸氧 47%,无创机械通气 50%,P=0.18)。
然而氧合指数<200mmHg的受试者中,高流量鼻导管吸氧组(35%)与常规面罩组(53%)或无创机械通气组(58%)相比较28天内插管率明显降低(P=0.01)。
此外,高流量鼻导管吸氧组(12%)与常规面罩组(23%)或无创机械通气组(28%)相比较90天内死亡率明显降低(P=0.02)。
高流量鼻导管吸氧的明显患者受益的可能解释包括无创机械通气组平均潮气量9
mL/kg对于患者来说相对较高和有潜在的损害、高流量鼻导管吸氧组小剂量气道正压可以增加CO2排出、总体气管插管率减少,而有研究已经证明气管插管是ARDS患者死亡率较高的危险因素。
2.机械通气气压管理策略的重要性数据的二次分析
过去15年来临床医生治疗ARDS患者的时候都在努力减少机械通气导致的肺损伤,努力在尽可能的最大程度的扩张肺泡的同时限制潮气量和平台压。
Amato和同事试图带领医生走出困境,进行二次数据分析驱动压对ARDS临床预后的作用。ARDS患者驱动压=平台压-PEEP。
这些研究人员综合分析几个ARDS通气管理的随机对照试验数据,使用复杂的统计方法(中介分析)分别计算潮气量、PEEP、平台压和驱动压对ARDS患者预后的作用。
研究得出结论,驱动压而非潮气量是ARDS患者预后的主要决定因素,可能因为ARDS患者大部分肺泡塌陷或水肿,目标驱动压可影响患者功能肺的有效潮气量。
虽然研究结果很有趣,但这些研究仍部分停留在假设阶段,没有足够的实质性证据,还需要随机对照试验进一步研究。
3.ARDS临床和生物异质性
今年两项新研究进一步增加人们对ARDS的临床和生物异质性的理解。
Jabaudon和同事分析sRAGE(soluble receptor for advanced glycation end products ,晚期糖基化终末产物可溶性受体)生物标志物和肺泡液体清除率之间的关联。
ARDS小鼠试验和临床试验结果显示血浆sRAGE浓度和支气管肺泡灌洗与肺泡液体清除率呈高强度反向相关,值得注意的是ARDS患者之间肺泡液体清除率存在明显差异,变化范围从几乎为零到基本正常。
生物标志物可以识别这种生物学或生理变化,或两者兼而有之,最终可能促进人类ARDS靶向治疗的发展。
Lorente和同事采取不同的方法进行试验,提出观点认为尸检结果显示ARDS患者存在DAD(diffuse alveolar damage ,弥漫性肺泡损伤)可以代表ARDS一个亚型。Lorente分析了两组ARDS尸检队列,指出伴有DAD的ARDS患者氧合指数、肺顺应性较低,更有可能死于低氧血症。
尽管这些结果为ARDS的临床和生物学异质性增加了证据,伴或不伴有DAD的ARDS患者对治疗的反应性是否不同—ARDS临床亚型的真正特点,目前仍不清楚。
4.肺再生医学研究
最后,再生医学的前景很有吸引力。内源性肺祖细胞理论上可以被用来修复受伤的肺泡上皮-毛细血管壁。
Vaughan和同事使用大鼠流感模型研究阴性品系肺上皮干细胞修复严重肺泡上皮损伤的作用。这些肺上皮干细胞细胞在小鼠流感损伤后原位生长,移行和后续分化成类似II型肺泡细胞和远端气道上皮组织,后续在修复相分化成异常的囊性结构。
Rosen和同事报道使用萘和辐射损伤小鼠,随后向小鼠体内移植人类或小鼠胚胎肺组织可以重建受体小鼠肺泡上皮结构。
鉴别出关键的人体肺祖细胞将是接下来重要的研究过程。
虽然这些治疗方法进入临床试验还需要许多年,已经有临床研究分析间充质干细胞在ARDS治疗中的潜在作用,临床研究人员对急性肺损伤后促进修复和增强肺再生的兴趣持续增长。
结语:理想情况下在接下来的十年中,这些研究方向将进一步扩大,集中在一起达到ARDS精准治疗的目标,识别每位ARDS患者特定的生物学和生理异常,提供有针对性的支持、修复和再生治疗。
Carolyn S Calfee报告接受美国NIH基金、社会捐款和GSK、Cerus Corp付款,Boehringer Ingelheim支付差旅费。
原始出处:
Carolyn S Calfee. ARDS in 2015: new clinical directions, new biological insights. Lancet Respir Med. December 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#呼吸病学#
30
#专题#
45
#RDS#
29
#呼吸病#
0
#Lancet#
35
好东西,值得分享,学习了!
107
好文章,值得收藏
153
好文章,值得收藏
139
#Med#
19