JAMA:长效支气管扩张剂或增加慢性阻塞性肺疾病患者心血管事件风险
2013-05-28 JAMA dxy
日前一项综述研究表明,两种用于慢性阻塞性肺疾病(COPD)的常用药物可引起心血管事件风险升高。研究结果5月21日在线发表于JAMA杂志子刊,它发现两种吸入式长效β受体激动剂(LABA)和长效抗胆碱能药物,新开具处方使用时与同类非处方药物相比,会引起心血管事件风险增加31%。 多伦多临床科学研究室Andrea Gershon医生及其同事考察了医疗保健数据库,并从中确认了191000余例接受5年以上
日前一项综述研究表明,两种用于慢性阻塞性肺疾病(COPD)的常用药物可引起心血管事件风险升高。研究结果5月21日在线发表于JAMA杂志子刊,它发现两种吸入式长效β受体激动剂(LABA)和长效抗胆碱能药物,新开具处方使用时与同类非处方药物相比,会引起心血管事件风险增加31%。
多伦多临床科学研究室Andrea Gershon医生及其同事考察了医疗保健数据库,并从中确认了191000余例接受5年以上治疗的66岁以上COPD患者。他们指出,在受试人群中,约有28%(53,532例)的患者因急性冠脉综合征(ACS)、心衰、缺血性卒中或心律失常而接受急诊或入院。研究中对所有COPD患者与非COPD患者进行匹配后方加以分析。
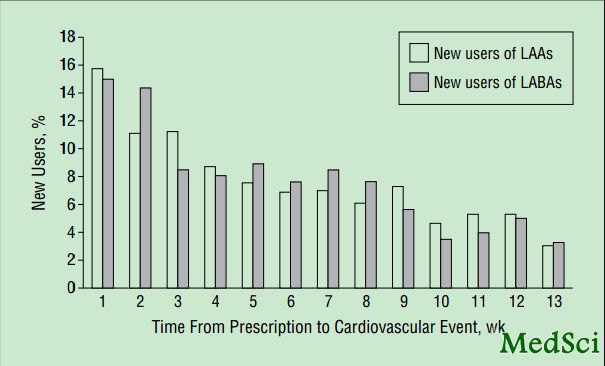
Gershon医生等人写道,研究发现,LABA和长效抗胆碱能药物在启用后2~3周内相关事件风险最高,并且药物之间未见差异。当对个体心血管终点进行单独评估时,研究者发现ACS和心衰风险升高,但心律失常和卒中风险并非如此。实际上,长效抗胆碱能药物对缺血性卒中有保护作用,但新LABA处方药则无此效应。
研究作者强调,长效支气管扩张剂与心血管事件之间的关系在POET-COPD随机对照研究以及之前的一项相同组别设置的小型研究得到证实。但加利弗尼亚大学Prescott G Woodruff医生在随刊述评中指出,其它试验和分析结果也同样给人以鼓舞。此外,他指出,该药被誉为COPD治疗的“肱股”,它们可以改善肺功能,呼吸困难,加重率以及生活质量。目前尚没有其他药理学途径可以延缓疾病进展,而该疾病在全世界许多国家已经成为致死率第三高的疾病。
希望与困难中前行的严密监测策略
Gershon 医生及其合作者声称,“这些结果支持对所有接受支气管扩张剂的COPD患者予以严密监测,不管是使用哪一种药物。”然而,就像是Woodruff指出的那样,严密监护尚未得到强烈推荐,因此,监测的重要性及能否得到切实推行,还取决于主治医师的响应。Woodruff总结道:“这篇文章的重要贡献在于它把医生和责任感和响应度提升到一个新的高度。”正在进行的TIOSPIR安全性研究或许可解释不同COPD治疗药物的相对风险。

Cardiovascular Safety of Inhaled Long-Acting Bronchodilators in Individuals With Chronic Obstructive Pulmonary Disease.
Abstract
IMPORTANCE Chronic obstructive pulmonary disease (COPD) is a common and deadly disease. Long-acting inhaled β-agonists and anticholinergics, first-line medications for COPD, have been associated with increased risk of cardiovascular outcomes. When choosing between the medications, patients and physicians would benefit from knowing which has the least risk. OBJECTIVE To assess the association of these classes of medications with the risk of hospitalizations and emergency department visits for cardiovascular events. DESIGN We conducted a nested case-control analysis of a retrospective cohort study. We compared the risk of events between patients newly prescribed inhaled long-acting β-agonists and anticholinergics, after matching and adjusting for prognostic factors. SETTING Health care databases from Ontario, the largest province of Canada, with a multicultural population of approximately 13 million. PARTICIPANTS All individuals 66 years or older meeting a validated case definition of COPD, based on health administrative data, and treated for COPD from September 1, 2003, through March 31, 2009. EXPOSURE New use of an inhaled long-acting β-agonist or long-acting anticholinergic. MAIN OUTCOME AND MEASURES An emergency department visit or a hospitalization for a cardiovascular event. RESULTS Of 191 005 eligible patients, 53 532 (28.0%) had a hospitalization or an emergency department visit for a cardiovascular event. Newly prescribed long-acting inhaled β-agonists and anticholinergics were associated with a higher risk of an event compared with nonuse of those medications (respective adjusted odds ratios, 1.31 [95% CI, 1.12-1.52; P < .001] and 1.14 [1.01-1.28; P = .03]). We found no significant difference in events between the 2 medications (adjusted odds ratio of long-acting inhaled β-agonists compared with anticholinergics, 1.15 [95% CI, 0.95-1.38; P = .16]). CONCLUSIONS AND RELEVANCE Among older individuals with COPD, new use of long-acting β-agonists and anticholinergics is associated with similar increased risks of cardiovascular events. Close monitoring of COPD patients requiring long-acting bronchodilators is needed regardless of drug class.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#扩张#
34
#支气管#
51
#阻塞#
43
#支气管扩张剂#
50
#疾病患者#
38
#血管事件#
38
#心血管事件风险#
50