JNI:厚朴酚能抑制引发炎症性脑损伤的关键蛋白
2012-03-23 MedSci MedSci原创
厚朴酚 小胶质细胞是大脑的第一道防线,它能不断寻找感染并将之击退。但过度活跃的小胶质细胞可能会导致大脑内的炎症反应失控,结果会导致神经元损伤。发表在Journal of Neuroinflammation杂志上的一项新研究显示和厚朴酚(HNK)通过KLF4能减少激活的小胶质细胞中促炎性细胞因子以及炎性酶的产生,KLF4已被证实能调节DNA。 国家脑研究中心、Manesar和印度的科学家们用脂多
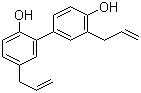
厚朴酚
小胶质细胞是大脑的第一道防线,它能不断寻找感染并将之击退。但过度活跃的小胶质细胞可能会导致大脑内的炎症反应失控,结果会导致神经元损伤。发表在Journal of Neuroinflammation杂志上的一项新研究显示和厚朴酚(HNK)通过KLF4能减少激活的小胶质细胞中促炎性细胞因子以及炎性酶的产生,KLF4已被证实能调节DNA。
国家脑研究中心、Manesar和印度的科学家们用脂多糖(LPS)刺激小胶质细胞的免疫反应。脂多糖能模拟细菌感染,小胶质细胞接受LPS刺激后开始行动,会释放炎性细胞因子如肿瘤坏死因子。
小胶质细胞活化也刺激一氧化氮(NO)和COX-2的生成,这些因子也导致炎症发生。然而,不受控制的炎症可导致神经元死亡和永久性脑损伤。在多数神经退行性疾病包括阿尔茨海默氏症、帕金森氏症和多发性硬化症中,小胶质细胞调控的炎症反应都有发生。
Anirban Basu博士领导的研究小组发现炎症反应由KLF4介导,KLF4是一转录因子,能直接与DNA结合以提高或阻碍基因的表达。用和厚朴酚处理小胶质细胞后,能降低其激活程度,同时LPS刺激细胞分泌的细胞因子也减少了。和厚朴酚也下调KLF4以及pNF-kb(另一种炎症调节因子)的活性。
Basu医生表示和厚朴酚下调KLF4后,结果会下调NO和COX-2的生成。他说:“和厚朴酚可以很容易地跨越血脑屏障,我们发现和厚朴酚不仅能减少pNF-kb和Klf4的水平,同时也能减少LPS诱导的老鼠大脑内激活的小胶质细胞的数量”。
他继续说,我们有关和厚朴酚的研究工作证实KLF4是一个重要的炎症调节因子。和厚朴酚和Klf4不仅在调节感染引发的炎症反应中起重要作用,也有可能在影响大脑和神经系统的其他疾病中有作用
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#关键蛋白#
36
#损伤#
29
#炎症性#
40