Lancet Oncol:艾瑞恩 vs 比卡鲁胺联合ADT治疗转移性激素阳性前列腺癌
2022-09-09 MedSci原创 MedSci原创
艾瑞恩 (瑞维鲁胺片,Rezvilutamide)是我国恒瑞自主研发的一种新型雄激素受体抑制剂,具有低血脑屏障渗透性,已显示出对转移性去势抵抗性前列腺癌的有效抗肿瘤活性。
艾瑞恩 (瑞维鲁胺片,Rezvilutamide)是我国恒瑞自主研发的一种新型雄激素受体抑制剂,具有低血脑屏障渗透性,已显示出对转移性去势抵抗性前列腺癌的有效抗肿瘤活性。
CHART研究旨在评估艾瑞恩 vs 比卡鲁胺联合雄激素剥夺治疗(ADT)在大体积、转移性、激素阳性的前列腺癌中的疗效和安全性。
这是一项在我国、波兰、捷克共和国和保加利亚的72家医院联合开展的随机、开放标签的3期研究,招募了年满18岁的ECOG表现状态0-1分的大体积、转移性、激素阳性的前列腺癌患者,随机(1:1)接受ADT联合艾瑞恩(240 mg/日)或比卡鲁胺(50 mg/日)治疗。主要终点是无影像学进展生存期和总生存期。
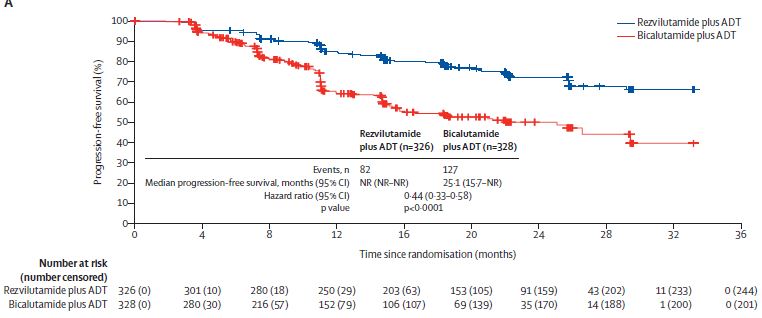
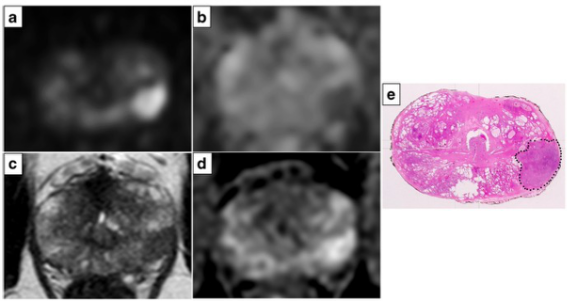
两组的无进展生存率
2018年6月28日-2020年8月6日期间,共筛查了792位患者,其中654位随机接受了艾瑞恩+ADT(n=362)或比卡鲁胺+ADT(n=328)治疗。截止2021年5月16日时(预定的中期分析),中位随访了21.2个月。与比卡鲁胺相比,艾瑞恩显著延长了患者的影像学无进展生存期(中位影像学无进展生存期:未达到 vs 25.1个月;HR 0.44, p<0.0001)。
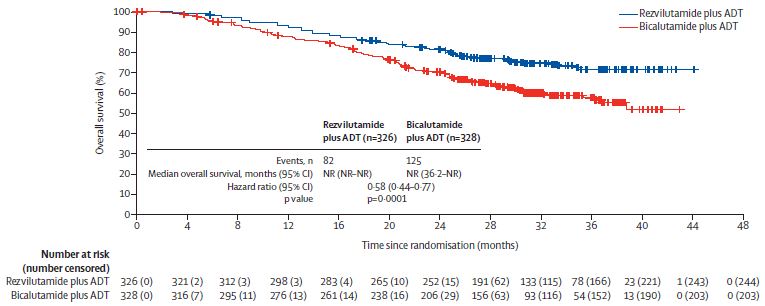
两组的总生存率
截止2022年2月28日,中位随访了29.3个月。与比卡鲁胺相比,艾瑞恩显著延长了患者的总生存期(中位总生存期均未达到;HR 0.58,p=0.0001)。
最常见的3级及以上的全因不良事件有高血压(艾瑞恩组 vs 比卡鲁胺组:8% vs 24%)、体重增加(6% vs 4%)、贫血(4% vs 5%)和低钾血症(3% vs 1%)。艾瑞恩组和比卡鲁胺组分别有90位和69位患者报告了重度不良反应。艾瑞恩组无治疗相关死亡;比卡鲁胺组有一例未知特殊原因的治疗相关死亡。
综上,与比卡鲁胺联合ADT治疗相比,艾瑞恩联合ADT显著延长了大体积、转移性、激素阳性前列腺癌患者的影像学无进展生存期和总生存期,且安全性可耐受。
原始出处:
Weijie Gu, et al. Rezvilutamide versus bicalutamide in combination with androgen-deprivation therapy in patients with high-volume, metastatic, hormone-sensitive prostate cancer (CHART): a randomised, open-label, phase 3 trial. Lancet Oncology. September 05, 2022. https://doi.org/10.1016/S1470-2045(22)00507-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
62
#Oncol#
53
#性激素#
66
#转移性#
66
#ADT#
66