Cell:沙门氏菌的天才生存指南
2015-02-05 佚名 生物谷
其实宿主免疫系统与病原体(广义:包括病变的自身组织)是一对哲上的矛盾。如果没有病原体的存在,免疫系统也就毫无意义。在进化过程中,宿主免疫系统与病原体在不断地调整自己,适应对方的特性,从而将自身的利益最大化。最近发表在《Cell:trends in immunology》杂志上的一篇综述类文章中,作者就沙门氏菌的感染方式与宿主的免疫策略做了系统的总结。 沙门氏菌是一类常见的寄生类微生物。最早见于美
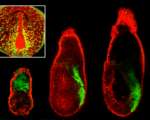
其实宿主免疫系统与病原体(广义:包括病变的自身组织)是一对哲上的矛盾。如果没有病原体的存在,免疫系统也就毫无意义。在进化过程中,宿主免疫系统与病原体在不断地调整自己,适应对方的特性,从而将自身的利益最大化。最近发表在《Cell:trends in immunology》杂志上的一篇综述类文章中,作者就沙门氏菌的感染方式与宿主的免疫策略做了系统的总结。
原始出处
Behnsen J1, Perez-Lopez A1, Nuccio SP2, Raffatellu M3.Exploiting host immunity: the Salmonella paradigm.Trends Immunol. 2015 Jan 9.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
43
#Cell#
36
已阅
108
已阅
116
#沙门氏菌#
49