Investigative Radiology:实现CT造影剂的“减价不减量”!
2022-09-06 shaosai MedSci原创
现阶段,临床上开发了多项技术以减少造影剂用量,重点是在减少造影剂用量的同时保留造影剂与噪声比(CNR)等图像质量参数。
 碘基造影剂(CM)是计算机断层扫描(CT)诊断中产生血管和软组织对比度的一个重要组成部分。然而CM不良反应种类繁多,包括过敏和类过敏反应、诱发甲状腺功能亢进症和剂量依赖性造影剂诱发的急性肾损伤。
碘基造影剂(CM)是计算机断层扫描(CT)诊断中产生血管和软组织对比度的一个重要组成部分。然而CM不良反应种类繁多,包括过敏和类过敏反应、诱发甲状腺功能亢进症和剂量依赖性造影剂诱发的急性肾损伤。
现阶段,临床上开发了多项技术以减少造影剂用量,重点是在减少造影剂用量的同时保留造影剂与噪声比(CNR)等图像质量参数。对比度可以通过调整注射方案参数(如CM和盐水注射速度)和调整CT扫描参数(如X射线管电压)来改变。最近,在人工智能方面的技术进步的背景下,可使用生成对抗网络(GAN)进行优化的虚拟对比度增强。在造影剂增强磁共振成像(MRI)的情况下,使用分割剂量的方法检测晚期造影剂阶段的脑转移,显示出高达90%的减少。然而迄今为止,还没有研究通过优化CT或MRI的虚拟造影剂增强来减少动态检查中多个CM阶段血管和实质的造影剂用量。
近日,发表在Investigative Radiology杂志的一项研究建立和验证了肝脏动态CT的优化虚拟对比度增强,在实验动物模型中使用GAN对真正的低CM和正常CM数据进行了评估,为在保证图像质量的同时进一步减少造影剂的使用提供了参考。
本研究使用20只健康的哥廷根迷你猪在3个不同的场合进行了低(低CM,105μL/kg)和正常(正常CM,350μL/kg)造影剂剂量的腹部低千伏CT(90kV)扫描,共120次检查。这些检查包括动脉早期、动脉晚期、门静脉和静脉期阶段。由于检查不完整,一只动物不得不被排除。19只动物中的3只被随机选择并用于验证(18项研究)。随后,用剩下的16只动物(96次检查)对GAN进行了图像到图像的转换,即从低CM到正常CM(虚拟CM)。为了验证,在腹主动脉、下腔静脉、门静脉、肝实质和自体背部肌肉中进行感兴趣区域测量,并计算对比度-噪声比(CNR)。此外,正常CM和虚拟CM的数据以视觉图灵测试的方式呈现给3位放射科医生。一方面,他们必须决定哪些图像是来自正常的检查。另一方面,他们必须评估这两张图像是否符合病理。
平均血管CNR(低CM 6.9 ± 7.0 vs 虚拟CM 28.7 ± 23.8,P < 0.0001)和实质(低CM 1.5 ± 0.7 vs 虚拟CM 3.8 ± 2.0,P < 0. 0001)CNR通过基于GAN的对比度增强在所有对比度阶段明显增加,与正常CM检查没有明显差异(血管:虚拟CM 28.7 ± 23.8 vs 正常CM 34.2 ± 28.8;实质:虚拟CM 3.8 ± 2.0 vs 正常CM 3.7 ± 2.6)。在视觉图灵测试中,放射科医生报告说,在96.5%的检查中,来自正常CM和虚拟CM的图像在中位数上是一致的。此外,在91%的病例中,检查者有可能将正常中医的数据识别为这样。
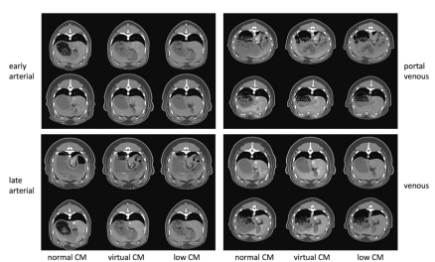
图 动脉早期(左上)、动脉晚期(左下)、门静脉(右上)和静脉(右下)造影剂阶段的低CM、虚拟CM和正常CM图像的例子。CM,造影剂
本项研究表明,使用基于GAN的多期肝脏CT增强扫描检查可在保证图像质量的前提下可以减少70%所需的造影剂量。
原文出处:
Johannes Haubold,Gregor Jost,Jens Matthias Theysohn,et al.Contrast Media Reduction in Computed Tomography With Deep Learning Using a Generative Adversarial Network in an Experimental Animal Study.DOI:10.1097/RLI.0000000000000875
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#EST#
120
非常棒
92
#造影#
121
#IgA#
108