术语
-
表现为血管母细胞瘤、透明细胞肾癌、囊腺瘤、嗜铬细胞瘤的常染色体显性遗传综合征
影像
-
两个或多个中枢神经系统血管母细胞瘤,或者一个血管母细胞瘤伴内脏病灶或视网膜出血
-
血管母细胞瘤大小各异,可从很小到非常大,可伴发更大的囊肿
主要鉴别诊断
-
血行转移癌
-
孤立的血管母细胞瘤
-
毛细胞性星形细胞瘤
-
十几岁或年轻成人的半球髓母细胞瘤
-
血管神经皮肤综合征中的多发性动静脉畸形
病理
-
血管母细胞瘤分布靠后部,是肿瘤发生在胚胎发育期的结果
临床要点
-
表型基于嗜铬细胞瘤的存在或缺失
-
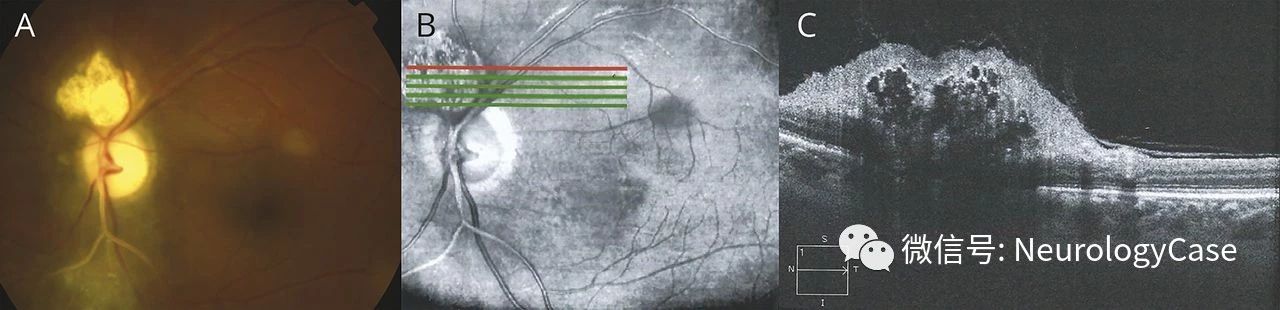
VHL最初表现为视觉症状
-
近75%产生症状的肿瘤有伴发的囊肿、瘤周水肿
诊断纲要
-
遵从NIH(美国国家健康研究院) 筛查标准(从11岁开始,每两年行脑脊髓增强MR、每年做腹部超声;20岁开始,每年或每隔一年做腹部CT;若听力丧失/耳鸣/眩晕行颞骨MR)
-
伴平衡障碍、听力丧失或耳胀的VHL患者, 应查找内淋巴囊肿瘤

-
彩图:VHL患者有2个血管母细胞瘤,位于脊髓的肿瘤伴发囊肿,有可能引起脊髓病,位于小脑较小的血管母可能为无症状性。
-
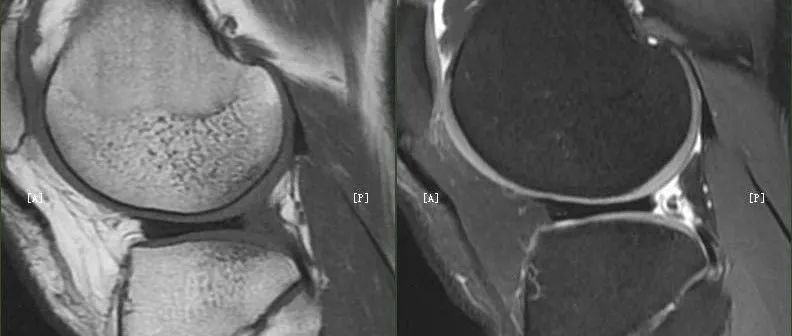
矢状位T1WI +C:颅颈交界区3个血管母细胞瘤,两个源于延髓背侧,伴发小囊肿;C4水平微小强化结节伴较大囊肿,严重压迫脊髓并使之增粗。
-
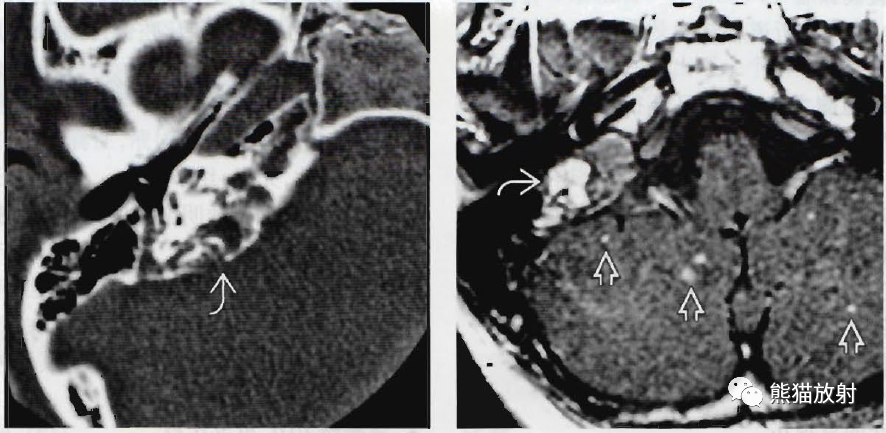
14岁VHL患者,轴位CT显示右侧岩骨内侧一破坏性肿块,内淋巴囊肿瘤,位于内淋巴囊和前庭导水管中央为此类病灶的共同特点。
-
轴位MR增强:同一位患者,内淋巴囊肿瘤为高信号,小脑多发微小强化结节,提示血管母细胞瘤。

-
42岁患者,轴位T2WI:典型的小脑半球血管母细胞瘤,有占位效应,瘤周轻度水肿。
-
同一位患者,囊肿下侧面可见明显强化的实性结节。
结节性硬化症
术语
-
结节性硬化症(TSC)
-
同义词:Bourneville-Pringle综合征
-
伴多器官错构瘤的遗传性肿瘤疾病
影像
-
室管膜下钙化小结节(错构瘤)
-
室管膜下巨细胞性星形细胞瘤;绝大多数位于室间孔(15%)
-
皮质或皮质下结节(95%)
-
白质放射状迁移线
-
囊样白质病灶(囊状大脑变性)
-
皮质或皮质下结节:早期T1WI高信号, 但髓鞘成熟后有变化
-
MR比CT更易看到室管膜下钙化小结节强化
-
AMT-PET可区分致癫痫性与非致癫痫性结节
主要的鉴别诊断
-
X-连锁室管膜下异位
-
巨细胞病毒感染:脑室周围钙化、常见白质病灶、多小脑回
-
Taylor型皮质发育不良(FCD 2型
病理
-
生发基质细胞分化/增生异常
-
TSC抑癌基因突变导致细胞分化和增生异常
诊断纲要
-
FLAIR和T1WI磁化传递成像诊断TSC最敏感
-
室管膜下钙化小结节(<1.3cm),室管膜下巨细胞型星形细胞瘤(>1.3cm)
-
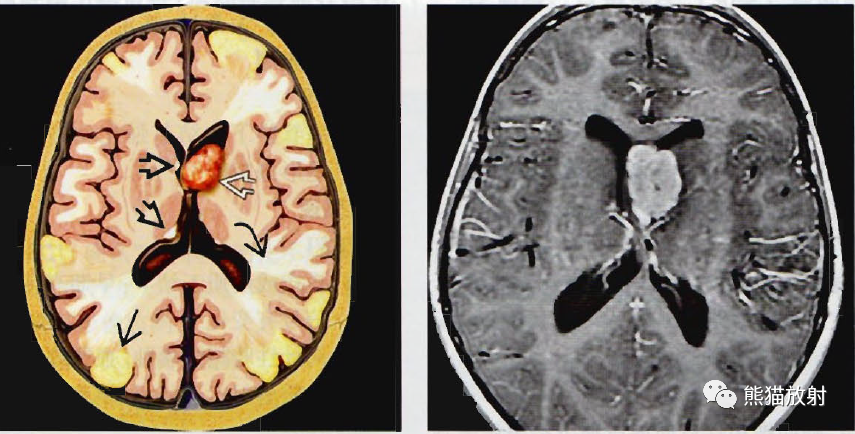
轴位示意图:TSC脑部受累,左侧室间孔有一巨细胞型星形细胞瘤(白空箭)、室管膜下小结节(黑空箭)、放射状迁移线(黑弯箭)或皮质/皮质下结节(黑直箭)。
-
轴位增强:室间孔处肿瘤明显均匀强化。
-
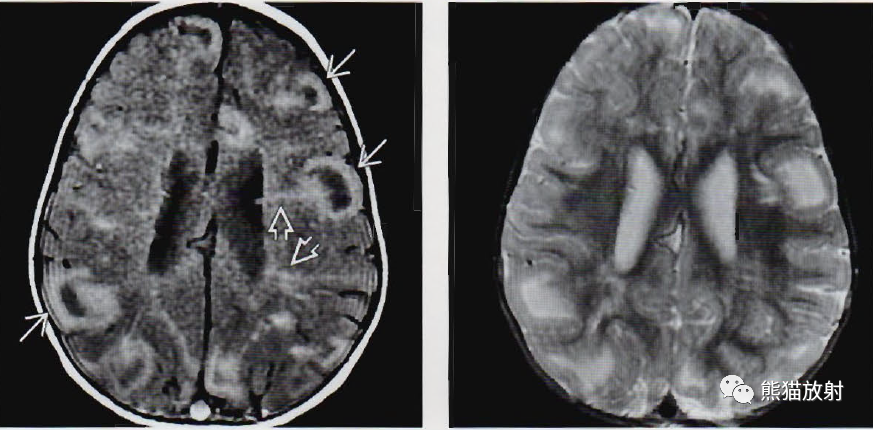
轴位T1WI和磁化传递成像显示13个月TSC患者的典型表现:多发皮质/皮质下结节和白质放射状迁移线。正常白质信号被磁化传递脉冲所抑制,故而这些病灶可以清晰显示。
-
同一患者,相应轴位T2WI显示扩张脑回下方有多个高信号的结节病灶,白质放射状迁移线显示不明显。
-
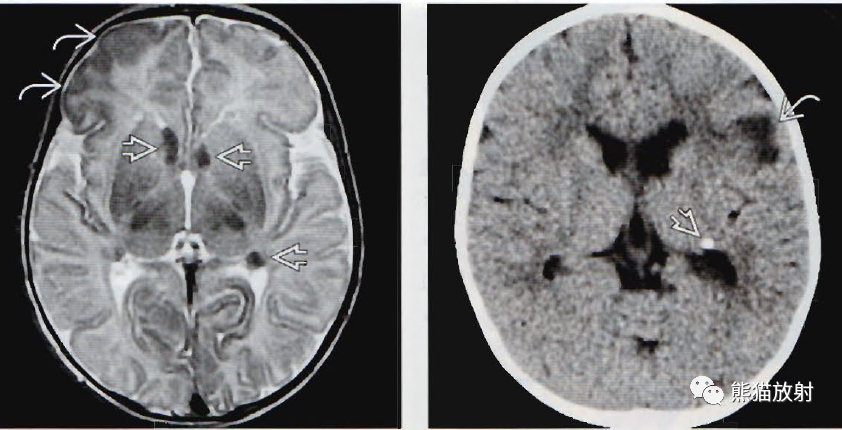
一个月大的患儿,轴位T2WI显示多个低信号室管膜下小结节,起源于侧脑室壁。右侧额叶皮层增厚。70岁NF2患者,轴位增强显示后颅窝多发脑膜瘤(直箭),双侧内听道神经鞘瘤。
-
另一患者,CT平扫显示左侧侧脑室室管膜下小结节钙化,左额叶低密度皮质下病灶。
内容节选自图书:《脑部影像诊断学》 主译:吴文平 等
整理来源:熊猫放射

如何保护孩子?父母要了解的医疗辐射安全常识

伍建林:胸部疾病影像学漏误诊分析与启示

这八句话,让医生怀疑人生......
超实用CT诊断测量方法与技巧(建议收藏)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#结节性#
49
#硬化症#
45
#VHL#
50
#综合征#
53
#临床诊断#
46
#诊断要点#
40