Clin Kidney J :干扰素-β治疗继发性肾脏疾病的意义
2022-02-18 从医路漫漫 MedSci原创
干扰素-β (IFN-β)相关肾病的病历仍然缺乏描述,这种不寻常关联的潜在特征仍有待确定。

背景:干扰素-β (IFN-β)相关肾病的病历仍然缺乏描述,这种不寻常关联的潜在特征仍有待确定。
方法:在本研究中,我们回顾性分析了活检证实的肾疾病患者接受IFN-β治疗至少6个月的临床、实验室、组织学和治疗资料。
结果:18名患者(13名女性,中位年龄48岁)在干扰素-b治疗期间经活检证实患有肾脏疾病。接受IFN-β治疗的患者(14例接受IFN-B1A治疗,4例接受IFN-B1B治疗)的中位暴露时间为67个月(23-165个月)。临床表现包括高血压(HT;83%)、恶性HT(44%)、蛋白尿(ProtU)>1g/g(94%)、肾功能降低(78%)、血栓性微血管病变(TMA;61%)、水肿综合征(17%)或肾病综合征(11%)。病理表现为孤立TMA 11例,孤立局灶节段性肾小球硬化(FSGS)2例,合并TMA和FSGS病变5例。对10例(63%)替代补体途径的探索没有发现调节补体系统的基因突变。统计分析强调,与干扰素-b相关的TMA的发生与REBIF显著相关,每周剂量>50毫克,并每周多次注射。在所有病例中,干扰素-β治疗均停止。TMA病变的患者接受其他治疗,包括皮质类固醇(44%)、eculizumab(13%)和血浆置换(25%)。在36个月的中位随访结束时,分别有61%和22%的患者观察到持续性HT和持续性protU。估计肾小球滤过率<60mL/min/1.73m2的患者占61%。
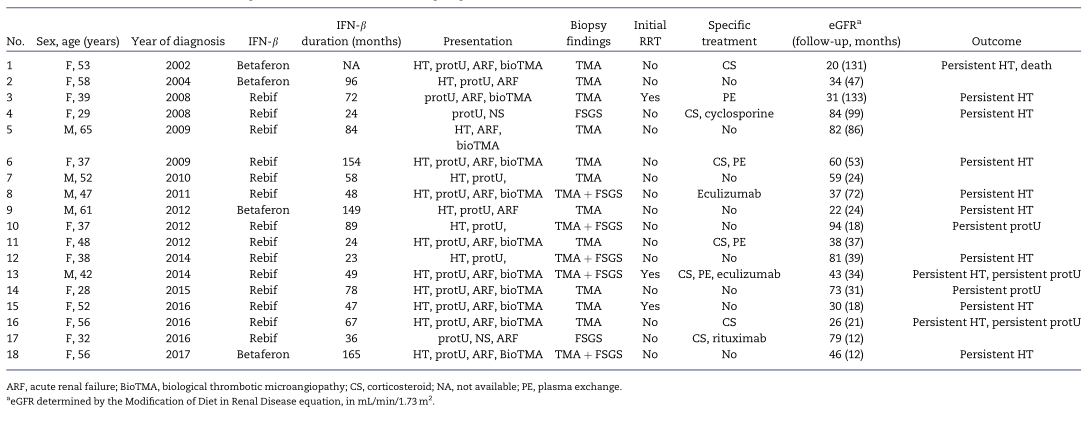
表1.18例干扰素-β相关肾病患者的临床表现和转归
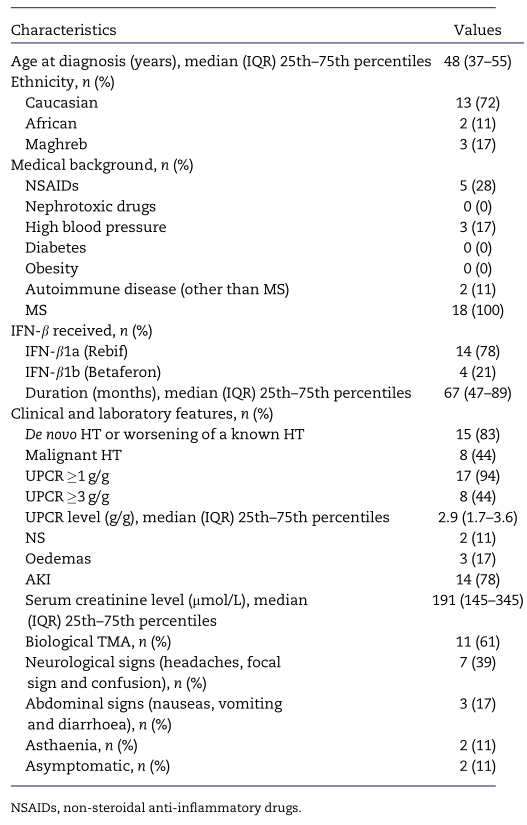
表2.18例干扰素相关肾病患者的人口学、临床和实验室特征
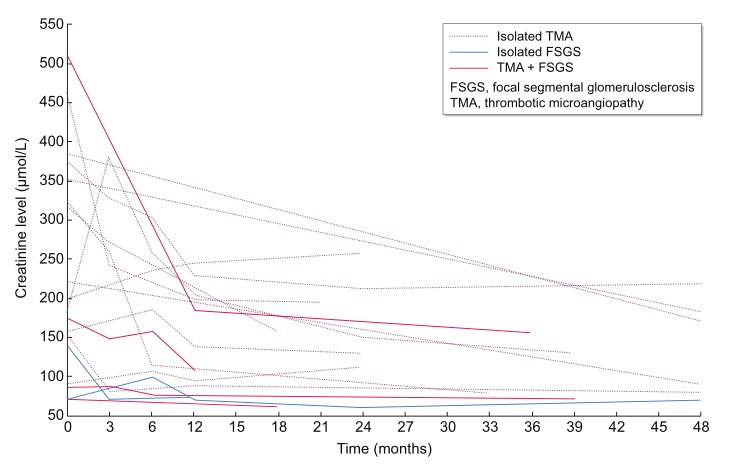
图1:随访期间肌酐水平的变化

表3.18例干扰素相关肾病的诊断和活检结果

图2 血栓性微血管病变。(A)低倍肾小球缺血(马森氏三色)。(B)高倍镜下肾小球血栓性微血管病变。(C)高倍镜下小动脉血栓性微血管病变。(D)肾小球血栓性微血管病变。
结论:在治疗过程中出现HT和/或ProtU时,必须考虑干扰素-β相关性肾病。当肾活检发现TMA和/或FSGS时,早期停用IFN-β是必要的。
原文出处:Dauvergne M, Buob D, Rafat C,et al.Renal diseases secondary to interferon-β treatment: a multicentre clinico-pathological study and systematic literature review.Clin Kidney J 2021 Dec;14(12)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#继发性#
39
#继发#
32
学习学习
37
#kidney#
34